COVID-19 Research
COVID-19 Research: Emory’s work spans the gamut, from bench to bedside
Within weeks after the pandemic began, researchers across a wide variety of disciplines at Emory University mobilized their resources and expertise to address various dimensions of COVID-19. Some researchers began anew while others pivoted from their existing work on emerging infectious diseases to address the new coronavirus.
The intricate tapestry of COVID-19 activities spans the spectrum of disease – from advancing understanding of the virus to coming up with quicker and more accurate tests to finding treatments and a vaccine. Emory’s work is well positioned to go from bench to bedside because of its outstanding researchers and facilities, which include one of the world’s largest national primate centers, state of the art research laboratories, and a comprehensive health system that can host clinical trials for the next lifesaving drug or vaccine.
The projects, at various stages of development, have received more than $61 million in federal grants so far, and include:
- Rolling out an ambitious vaccine trial sponsored by the National Institute of Allergy and Infectious Diseases (NIAID) that launched in record speed
- Enrolling more patients in a global antiviral therapeutic trial that preliminary data has shown helped hasten recovery for certain patients and subsequently, launching a second arm of that trial which combines the antiviral with an anti-inflammatory drug
- Receiving the largest award from the National Institutes of Health (NIH) in a single budgetary year to rapidly create widely accessible diagnostic tools and tests
- Building a national, county-level dashboard and tracking map that will enable local officials to understand epidemiological trends and respond accordingly
- Helping implement a national seroprevalence survey to understand how many adults in the U.S. have antibodies to the virus
CLINICAL TRIAL
Emory is testing a vaccine candidate as part of NIH's first such clinical trials against COVID-19 in the United States. Emory is currently one of three sites in the U.S. for the trials, funded by the NIH's National Institute of Allergy and Infectious Diseases (NIAID). Preliminary results have been encouraging. The trials are expected to move to phase 3 in July, where the vaccine will be administered to thousands of eligible participants and tested for safety and efficacy. The vaccine consists of an RNA molecule and like many of the other SARS-CoV-2 vaccines in development, it is designed to train the immune system to make antibodies that recognize and block the spike protein that the virus uses to enter human cells.
Investigators: Drs. Evan Anderson, Nadine Rouphael, David Stephens, Emory Vaccine Center researchers
IN PROGRESS
Researchers have received a two-year grant from the NIAID to develop a MVA-based vaccine for SARS-CoV-2. The team is using its expertise with developing an MVA-based vaccine for HIV/AIDS, which recently successfully completed phase 2 clinical trials in the United States. A single MVA vaccination has been shown to provide protection against multiple viral infections, including another coronavirus, SARS, Zika, and Ebola. Another major advantage of MVA vaccines is that they can be used in combination with other vaccines to enhance the immune system's response.Investigators: Drs. Rama Amara, Mehul Suthar
IN PROGRESS
Emory researchers are evaluating novel adjuvants that can help produce more effective vaccines. Adjuvants are stimulants in the vaccine that can significantly accelerate the speed, quantity and longevity of the body's ability to make virus neutralizing antibodies. Vaccine studies in nonhuman primates are scheduled to start soon. The durability of antibody responses and other immune responses will be systematically investigated.Investigators: Drs. Sudhir Pai Kasturi, Mehul Suthar
IN PROGRESS
Public health researchers are investigating models for optimal COVID-19 vaccine strategies. This work will help inform both direct protection and herd immunity benefits of various COVID-19 vaccination approaches.Investigators: Dr. Ben Lopman
IN PROGRESS
Emory is part of a global network of NIH sites that is testing remdesivir, an antiviral that has shown promise for certain categories of hospitalized patients for the new coronavirus. The FDA has approved emergency use of the drug and researchers will continue to evaluate longer-term impact of the drug. Emory is also part of the next iteration of this study that is investigating the effectiveness of remdesivir with the anti-inflammatory drug, baricitinib. (see below)
Investigators: Drs. Aneesh Mehta, Nadine Rouphael, Emory Vaccine Center ID faculty
IN PROGRESS
Emory is part of an international study combining baricitinib and remdesivir as a new treatment strategy. Baricitinib is an oral, anti-inflammatory drug already approved by the FDA for rheumatoid arthritis. Remdesivir is an experimental antiviral medication administered by infusion, which means it can be given only to hospitalized patients. This COVID-19 combination study will explore baricitinib's ability to calm the hyper-inflammatory response (also called cytokine storms) that the disease causes in the lungs and determine whether the drug is best used alone or in combination with remdesivir. Cytokine storms, which can be triggered by auto-immune conditions or infections such as the flu, describe an immune response where the body starts to attack its own cells and tissues rather than just fighting off the virus. The trial will randomly assign eligible participants to one of two treatment arms: one group will get the combination therapy of baricitinib+remdesivir while another will receive a placebo and remdesivir.
In addition to the baricitinib study, researchers have launched another double-blind, randomized, placebo-controlled trial with an immunomodulator called imatinib or nilotinib to limit hyper-inflammatory responses characteristic of severe COVID-19 disease.
Investigators: Drs. Vincent Marconi, Nadine Rouphael, Ray Schinazi, Marshall Lyon, Michael Hart, Daniel Kalman, Emory ID faculty
CLINICAL TRIAL
Researchers at Emory have found that nearly all people hospitalized with COVID-19 develop virus-neutralizing antibodies within six days of testing positive. The research focused on patients' antibody response during hospitalization; most other studies on the topic have focused on the immune response after hospitalization. Testing for neutralizing antibodies is more time-consuming than other antibody tests and must be done in a biosafety level 3 laboratory which Emory possesses.
The study's findings have implications for convalescent plasma therapy and vaccine development. Using this research, clinicians will evaluate the use of convalescent plasma with high levels of neutralizing antibodies as a treatment for the new coronavirus. The U.S. Food and Drug Administration has approved the use of convalescent plasma therapy as an experimental treatment in clinical trials and for critically ill COVID-19 patients.
Emory is expected to be a clinical trial site for an antibody therapy from pharmaceutical Eli Lilly, LY-CoV555. It is the first potential new medicine specifically designed to attack SARS-CoV-2, the virus that causes COVID-19.
Investigators: Drs. John Roback, Sean Stowell, Colleen Kraft, Nadine Rouphael, Aneesh Mehta, Rafi Ahmed, Jens Wrammert, Mehul Suthar
CLINICAL TRIAL
Emory researchers are involved in a multi-center, adaptive, randomized, double-blind, placebo-controlled study to assess the efficacy and safety of gimsilumab, a human monoclonal antibody, in patients with lung injury or acute respiratory distress syndrome due to the new coronavirus. Researchers have received a grant from Kinevant Sciences, which is part of the pharmaceutical that makes the drug compound.
Researchers have also begun to identify useful antibodies in patients infected with the new coronavirus to produce clones that can be used to help critically ill patients. Monoclonal antibodies have been used successfully by Emory experts in patients with H1N1 and Ebola.
Investigators: Dr. Marshall Lyon; Drs. Jens Wrammert, Carl Davis
IN PROGRESS
Merck has brought rights to an antiviral compound that was discovered at Emory. EIDD-2801 was invented by Drug Innovation Ventures at Emory (DRIVE), a not-for-profit biotech which partnered with privately held biotech, Ridgeback Biotherapeutics, to rapidly advance drug development. The agent was effective against previous coronaviruses such as MERS and SARS. An oral therapeutic could reduce transmission as it is likely that infected people would not be contagious after a short course of an effective drug.
DRIVE leads: Drs. George Painter, Dennis Liotta
IN PROGRESS
Emory University researchers are leading a NIAID-funded multi-site study across the United States to track the immune responses of people hospitalized with COVID-19 that will help inform how the disease progresses and potentially identify new ways to treat it. The research will determine how certain immunological measures correspond to or even predict the clinical severity of COVID-19.
Investigators: Dr. Nadine Rouphael
IN PROGRESS
Emory is identifying immune biomarkers of SARS-CoV-2 by infecting primary and cultured human lung cells as well as human tissues with the new coronavirus to understand host response to the virus. What happens once the lung cells are infected could shed light on the inner workings of the virus that causes covid-19, and how the body is reacting to it. This investigation could help zero in on where the damage is worst. Researchers working on these lung models will also be better able to understand how particular cell types react to infection and that could potentially help identify optimal intervention pathways for therapies.
Investigators: Drs. Mehul Suthar, Anice Lowen. Larry Anderson, Jake Kohlmeier, Steve Bosinger
IN PROGRESS
Researchers are studying monoclonal antibodies from lampreys to better understand the new coronavirus. Lampreys are an ancient species of fish resembling eels and provide important clues for researchers about the evolution of our immune system, and potential ways to fight new pathogens. The monoclonal antibodies produced by this project will be used for virus isolation and diagnosis, and could support the work of other researchers on campus to develop therapies.
Investigators: Drs. Max Cooper, Masayuki Hirano
CLINICAL TRIAL
A research team is using low dose radiation therapy (LD-RT) to treat COVID-19 patients to reduce the pulmonary inflammation that severely affects these patients and threatens their ability to breathe on their own. The first cohort in this Phase I/II trial will consist of five critically-ill hospitalized patients not currently on ventilators, and it is hoped that the LD-RT will reduce their risk of requiring mechanical ventilation.
Investigators: Drs. Mohammad K. Khan, Clayton B. Hess
IN PROGRESS
Researches are using artificial blood vessel technology that was developed at Emory to determine “what goes wrong” in the circulation of the lungs when COVID-19 patients develop respiratory failure. They will perfuse blood from COVID-19 patients into microvasculature-on-a-chip systems, which will function like “vascular avatars” and could provide important information about the pathophysiology of COVID-19.
Investigators: Drs. Wilbur Lam, Greg Martin
IN PROGRESS
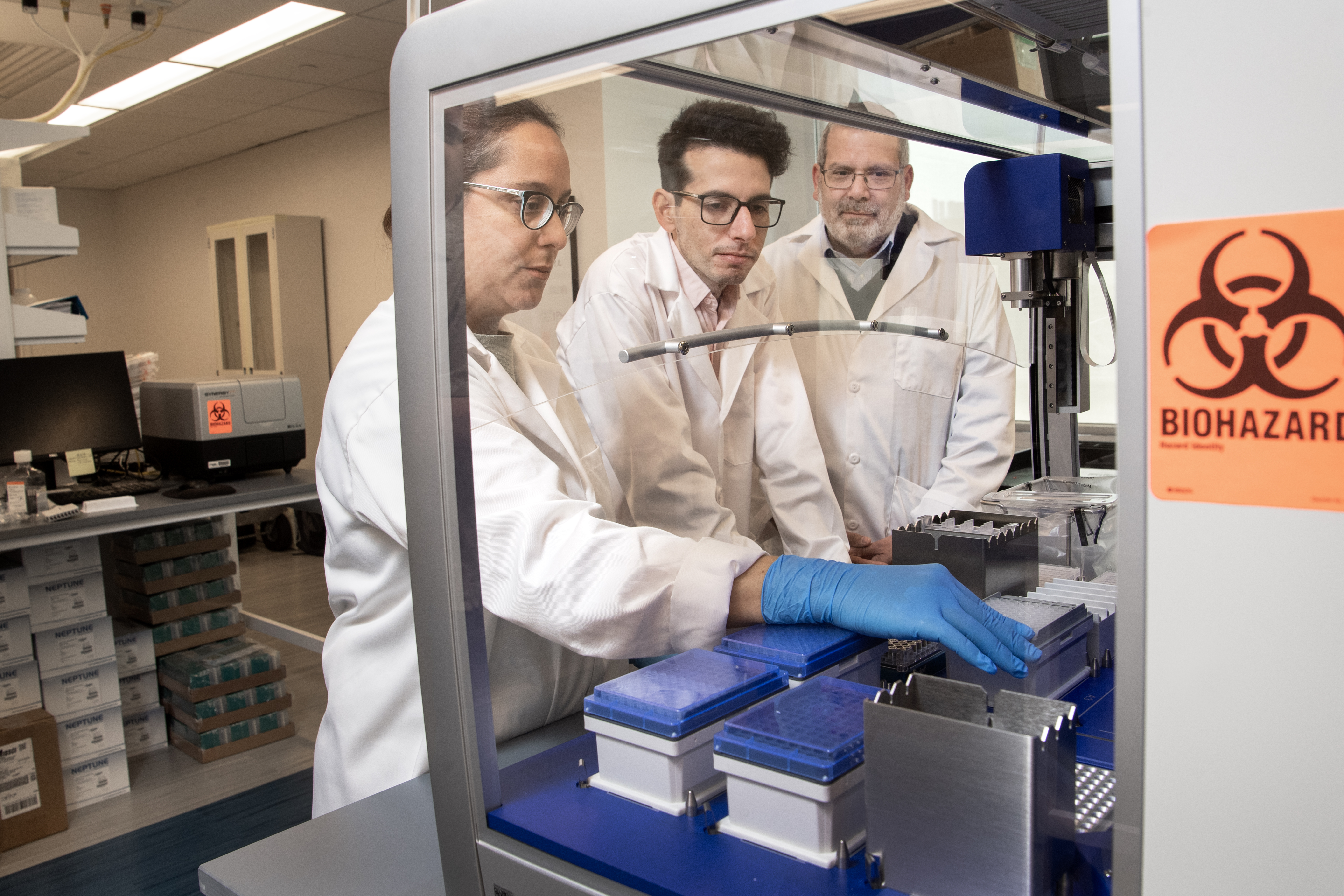
Emory is developing a test to screen millions of compounds (including FDA-approved drugs) and identify those that could block viral entry. The challenge is to quickly identify drugs that can interfere with this process—either existing medications that can be repurposed or potential new treatments that can be developed. The research team is creating the scientific tools needed to find these drugs, including a sophisticated, robot-enabled laboratory test to find possible candidates.
Investigators: Drs. Haian Fu, Joshy Jacobs
IN PROGRESS
Researchers are working with collaborators at the National Institutes of Health to study the Cystic Fibrosis Transmembrane Conductance Regulator (CFTR) gene as it may play a role during several key aspects of COVID-19 pathogenesis, including viral entry.
Investigators: Drs. Eric Sorscher, Stefan Sarafianos
IN PROGRESS
Apart from anti-inflammatories, researchers are repurposing drugs that have been approved for one indication and testing their ability to safely mitigate the harmful effects of the new coronavirus. A handful of marketed drugs show antiviral activity in cell culture for COVID-19, and in animals infected with MERS and SARS, which are coronaviruses similar to COVID-19. Since the drugs work at different points in the viral life cycle, it is reasonable to test these drugs in combinations to see which combinations might be particularly effective. Data on effective combinations could be immediately translated to treating humans infected with COVID-19 because the drugs are already on the market, widely available, and inexpensive. Moreover, drug combinations might allow for lower individual drug doses, thus decreasing potential side effects. These drugs will also be tested in combination with other antivirals such as remdesivir.
Investigators: Drs. Joshy Jacobs, Vikas Sukhatme
IN PROGRESS
The vast majority of COVID-19 fatalities can be attributed to dysfunction in the cardiovascular system. This is not due to heart attacks but most likely occurs as a result of a COVID-induced “cytokine storm” where multiple inflammatory proteins attack the heart and blood vessels and impair the ability of the heart muscle cells to contract. It is also clear that the virus can directly infect the heart muscle and blood vessel cells. In addition, the primary respiratory problem affecting COVID-19 patients often occurs as a result of dysfunction of the blood vessels in the lungs, resulting in fluid leaking into the lungs. Several cross-disciplinary teams are utilizing Emory's significant heart and vascular research expertise to engage in studies in humans and animal studies to quickly find solutions to prevent and treat these acutely ill patients.
Investigators: Emory researchers
IN PROGRESS
Emory researchers are leading a study to identify blood tests that can help determine which COVID-19 hospital patients are at the highest risk for developing blood clotting disorders that cause stroke, heart attack, or clots in the lungs, legs, or arms. Preliminary studies suggest that blood tests can identify these high-risk patients early and, with early use of blood thinning medications, can prevent clotting complications from the virus as well as improve survival. Another study is looking to understand why an enzyme that causes clotting becomes dysregulated during the course of the infection, which can be especially harmful to patients with pneumonia who are at high risk for respiratory failure and require in extreme cases, an artificial lung. Both projects will provide new insights into strategies for preventing blood clots which have been seen in around a third of patients of all ages who become ill with the virus.
Investigators: Emory stroke, neurology and heart and vascular researchers
IN PROGRESS
Researchers are working on experimental primary airway epithelial cell models to be used for the development of therapeutics for COVID-19.
Investigators: Drs. Eric Sorscher, Stefan Sarafianos
IN PROGRESS
Emory is one of three Atlanta institutions selected for a new $1.5 billion NIH initiative to rapidly transform new technology into widely accessible diagnostic tools for virus detection so that testing can be readily available to Americans this fall. Emory University School of Medicine Department of Pediatrics, Children's Healthcare of Atlanta and the Georgia Institute of Technology are teaming up for this initiative. The $31M funding for this project is the largest ever NIH grant that Emory has received in a single budgetary year. Researchers hope to have a point of care diagnostic by year's end.
Investigators: Drs. Wilbur Lam, Greg Martin and Oliver Brand
LAUNCHED
Emory has developed a SARS-CoV-2 antibody test to enhance disease detection. Antibody or serological tests can help answer critical questions such as disease progression in populations, exposure to the virus and infection spread. Antibody tests vary in accuracy. Emory's antibody test identifies the exact type of antibody that prevents the COVID-19 virus from connecting with and entering human cells, which allows physicians to better predict whether someone with a positive antibody test result is likely to be protected from future infection. Emory experts are also evaluating devices that collect plasma samples from blood droplets—taken by a finger prick—which can be transported safely through the mail/courier to Emory Medical Labs for the Emory antibody test. This innovation would combine “point of care” testing, which is convenient but less informative than needed, with the rigor of Emory's antibody test. To facilitate widespread antibody testing in the state, a reliable device for at-home sample collection is important. Furthermore, considering the supply chain challenges Georgia faced during the first wave of the pandemic, there is keen interest in homegrown antibody tests that bypass the reagents for which the rest of the world is competing. A team from Emory and the University of Georgia met in May to compare locally generated tests.
Investigators: Drs. John Roback, Jens Wrammert
LAUNCHED
Researchers have developed an in-house diagnostic testing for SARS-CoV-2 by expanding the existing nucleic acid tests. Test refinements are ongoing.
Investigators: Drs. Colleen Kraft, Babiker Ahmed, Mehul Suthar, Jesse Waggoner
IN PROGRESS
Investigators are fast-tracking the development of a COVID-19-specific multiplex MENSA test using 14 COVID-19 antigens for early diagnosis of acute infection. The COVID-19 MENSA test will be applied to: 1) symptomatic patients under investigation (PUI); 2) Early prognostication of severe COVID-19 infections; 3) identify resolution of infectivity and ongoing immune protection. Combined with serological testing, this approach can be applied to large scale testing of the healthcare workforce and determine eligibility and safety to return to work.
Investigators: Dr. Frances Eun-Hyung
IN PROGRESS
A low-cost, rapid, and accurate point of care diagnostic for RNA viruses would eliminate current barriers to performing molecular tests in many settings. Emory researchers, in collaboration with a group at Arizona State, are in the process of submitting funding to develop what they have termed the STRIKE platform. The platform is aimed at identifying emerging pathogens. This technology is notable in that it can be performed at room temperature without the need for enzymes, and production costs, at scale, would be far lower (in the order of a dollar) than current technologies. This could make molecular testing, the most accurate method in the acute phase, feasible just about anywhere.
Investigators: Drs. David Myers, Jesse Waggoner
IN PROGRESS
Researchers are investigating simple and inexpensive methods to test for SARS-CoV-2 that leverages existing technologies and testing platforms. The current pandemic has demonstrated the limitations of current mechanisms for assay roll-out, where central facilities are rapidly overwhelmed by test volume and assays implemented at individual sites are inconsistent in reliability and accuracy. This lag time between outbreak identification and access to accurate, standardized diagnostics has contributed to our inability to contain and manage the pandemic effectively. Researchers are seeking to develop protocols that address known limitations to existing molecular-based tests in use. The goal of this project is to develop a low cost and standardized molecular protocol that will be easy and safe to deploy, at room temperature, to areas with limited access, due to travel bans, and with scant laboratory resources.
Investigators: Dr Jesse Waggoner
IN PROGRESS
There is increasing evidence that the loss of smell is a presenting symptom in an otherwise asymptomatic disease. Researchers are hoping to study that and also define the role of smell testing as a screening measure in future diagnostic tools for COVID-19. Separately, public health researchers are building on previous work exploring the pathophysiological mechanisms by which coronaviruses affect the olfactory system to understand the impact of COVID-19 on the sense of smell.
Investigators: Drs. Josh Levy, Brad Pearce
LAUNCHED
Emory doctors have collaborated with Vital, a digital platform for the emergency department, on a COVID-19 symptom-checking app to help reduce the flood of patients to hospitals.
Developers: Drs. Alex Isakov, David Wright
LAUNCHED
The TechTank smartphone app does double duty as a symptom checker and contact tracer for COVID-19, and has been piloted in select hospitals. The app and companion website give health care facilities positive screening counts by zip code so they can identify “hot spots” for the disease and adjust operational plans accordingly.
Investigators: Drs. Charles Moore, Hope Bussenius
IN PROGRESS
A smartphone app that will use a suite of analytical tools to triage patients who suspect they've been infected, and also help continuously monitor potential worsening of symptoms through telemedicine. Meta-data from the app will be used to identify emerging hotspots and facilitate earlier targeted response. Initial sketch of app architecture is complete, and work is underway to move this to the next stage. Emory researchers are working with colleagues at the Georgia Tech Research Institute on this initiative.
Investigators: Drs. Rishikesan Kamaleswaran, Alessio Medda and colleagues at the Georgia Tech Research Institute
IN PROGRESS
Researchers are developing a privacy-enhanced real-time contact tracing app. The proposed app will guard the personal information of individuals who choose to use it, while also allowing them to monitor their risk of exposure to the virus that causes COVID-19. Anonymous users will be able to control and refine how frequently their data is captured and the amount of detail in the data. The research team is investigating additional protocols, such as encryption, for further privacy enhancement and will explore privacy-preserving mechanisms to share the collected data for research studies. Additional collaborators are at the University of Southern California and the University of Texas Health Science Center.
Investigators: Drs. Li Xiong, Vicki Hertzberg, Lance Waller
IN PROGRESS
Using physiological data such as heart rate variability from seriously ill COVID-19 patients, researchers are harnessing the power of artificial Intelligence to predict poor outcomes for ICU patients with the disease. Researchers have drawn information from a variety of sources, including patient monitors at ICUs across the Emory hospital system, to identify early signs of deterioration. Data was generated for 25 critically ill COVID-19 patients and then the forecasts were validated among 150 patients. This presents opportunities for novel, life-saving interventions and can further understanding of high-risk biomarkers. The goal is to create an algorithm that can then be used in the ER – and potentially, at some point in homes – to spot early signs of patients in distress.
Investigators: Drs. Rishikesan Kamaleswaran, Tim Buchman, Ofer Sadan, Prem Kandiah, Jim Blum
IN PROGRESS
Increased wait times in the emergency department increases the risk of infection transmission. Emory researchers are working on an open-source, low cost, non-invasive clinical screening system that will help health care providers automatically triage patients in EDs. The system initially focuses on two symptoms of the infection - fever and cyanosis. The use of visible infrared cameras allows for rapid assessment at a safe distance, reducing the load on medical staff and lowering the risk of spreading the infection within hospitals. Its clinical utility can be extended to non-emergency times as well to reduce wait time, channel the time and effort of healthcare professionals to more critical tasks, and also prioritize severe cases.
Investigator: Dr. Gari Clifford
IN PROGRESS
Investigators are looking at how COVID-19 infection in cells impacts certain proteins at a systemic level to develop high-throughput assays for diagnostics at both the symptomatic and asymptomatic stages. Another related study is using high-throughput screening to target the new coronavirus' protein interaction with host receptors to discover barriers to entry.
Investigators: Dr. Nicholas Seyfried; Drs. Haian Fu, Dennis Liotta
LAUNCHED
Emory experts have made available a text mining web-based tool for extracting and summarizing biological concepts e.g., diseases, species, mutations etc., in COVID-19 scientific literature. The searchable repository is dynamically updated and can help the scientific community answer high-priority questions related to COVID-19. Further, it will allow biomedical researchers and the general public to find information related to risk factors of COVID-19 including pregnancy, smoking, and comorbidities.
Investigator: Dr. Karen Uppal
IN PROGRESS
Researchers have built a dynamic and interactive web-based dashboard that displays the interplay between social determinants and COVID-19 epidemiological metrics at the county level. The dashboard is a public-facing tool that curates, disseminates and ultimately synthesizes actionable information to guide localized response to the epidemic over time. The dashboard allows users to quickly compare each county's COVID-19 cases, deaths, and social characteristics to the state and national average; visualize the relationship between social determinants and COVID-19 outcomes; view a printer-friendly report of detailed county data; and create side-by-side maps comparing key metrics at the county level. It also provides guidance on interpretation of displayed measures.
Investigators: Drs. K.M. Venkat Narayan, Shivani Patel
IN PROGRESS
Public health researchers are working on a national probability survey of active infections and seropositivity, to understand how many adults in the United States without a confirmed history of COVID-19 infection have antibodies to the virus. The presence of antibodies in the blood indicates a prior infection. Findings from this “serosurvey” will help illuminate the extent to which the novel coronavirus has spread undetected in the United States and provide insights into which communities and populations are most affected.
Investigators: Drs. Patrick Sullivan, Aaron Siegler
IN PROGRESS
A research team is conducting national surveys to assess public knowledge, attitudes, and practices related to physical distancing; perceptions about governmental response to the pandemic; disease testing; and willingness to receive a COVID-19 vaccine should one become available. This information will help guide decisions about a future vaccination program and a possible second wave of COVID-19 transmission.
Investigators: Dr. Bob Bednarczyk
IN PROGRESS
Researchers are modeling the use of serological tests as a complement to social distancing. Using a dynamic transmission model, they are evaluating the epidemiological consequences of selectively releasing people from social distancing based on their test results. A previously-planned study on social mixing patterns among U.S. office workers has been accelerated and is currently being implemented among participants in a number of corporate offices and one Emory University building. Partners on these projects include Georgia Tech and Yale University.
Investigators: Dr. Ben Lopman
IN PROGRESS
Researchers are developing machine learning models for forecasting Acute Respiratory Distress Syndrome (ARDS) among patients with the new coronavirus. Preliminary data shows that ARDS is linked to more than half of COVID-19 deaths. The models, which are being built from the records of more than 40 patients with ARDS, will enable early prediction of ARDS, somewhere between eight and 24 hours before it develops.
Investigators: Drs. Rishikesan Kamaleswaran, Greg Martin, Annette Esper
IN PROGRESS
Researchers are developing a transmission model for COVID-19 in cruise ships where close social interactions aided transmission. They will evaluate the effectiveness of different behavioral changes (social distancing, isolating, masking, frequent hand washing) in curbing transmission in such environments, and also apply the model to other densely populated settings such as nursing homes, college dorms, etc.
Investigators: Dr. Samuel Jenness
COMPLETE
In a collaborative study, Emory researchers looked at the racial disparities in COVID-19 cases and deaths across the United States. The study shows that counties with predominately black populations account for nearly 50 percent of all COVID-19 cases and more than 50 percent of COVID-19-related deaths.
Investigators: Drs. Patrick Sullivan, David Benkeser
IN PROGRESS
An estimated 25 to 50 percent of all deaths from COVID-19 in the United States have occurred among nursing home residents or employees, and even the strictest measures have not slowed the spread of the virus. Mathematical models using specific data are key to developing effective response plans. A Rollins research team is generating nursing home data needed to understand and reduce disease transmission.
Investigators: Emory Rollins School of Public Health faculty
IN PROGRESS
Emory researchers developed the EpiModel software, which provides tools for external researchers to model transmission and other dynamics of infectious diseases. It is currently being used by several research groups to model COVID-19.
Investigators: Dr. Samuel Jenness
IN PROGRESS
Following strict privacy safeguards, researchers will use the symptom checker app launched at Emory to create a nationwide cohort of 60,000 people who reported COVID-19 symptoms for several purposes including: 1. Determine whether the symptom tracker reduced healthcare utilization; 2. Clarify transmission patterns and explore how these patterns relate to outcomes and health care resources; and 3. Create a repository of data from the COVID-19 symptom tracker for Emory researchers to use for future grant submissions.
Investigators: Drs. Rachel Patzer, Justin Schrager
IN PROGRESS
Emory's infrastructure and scientific and technical expertise is being tapped during this pandemic to develop a validated non-human primate model to study the virology, immunology, and immunopathogenesis of COVID-19 and to test specific antibodies, vaccines, and antiviral compounds. Researchers are also conducting detailed and cutting-edge studies, in both humans and animal models, to determine specific features of the immune response to the new coronavirus disease.
Investigators: Drs. Mirko Paiardini, Thomas Vanderford, Anne Piantadosi, Steve Bosinger, Ray Schinazi, Guido Silvestri, Rabindra Tirouvanziam
IN PROGRESS
Investigators from Emory are leading a project to model the potential transmission dynamics of SARS-CoV-2 in wild apes. Previous studies have established that wild apes are highly susceptible to human respiratory diseases, but it is unknown whether the morbidity and mortality associated with SARS-CoV-2 in humans is similar in apes. All great apes are endangered and the majority are critically endangered, so if SARS-CoV-2 enters great ape populations, it may have the potential to lead to extinction events. To guide conservation and management of these endangered species at sites across Africa and Asia during the pandemic, the researchers will look at variables in potential transmission, from the ape population level to ecological interactions at the community level, including humans and other primate species. Collaborators include is RTI and the University of Nottingham.
Investigators: Dr. Thomas Gillespie
IN PROGRESS
Longitudinal study of pediatric health care workers to assess levels of positive IgG – a major antibody player that in its various forms provides the bulk of antibody-based immunity against invading pathogens. The study is framed on the hypothesis that pediatric health workers have a high prevalence of antibodies and if true, may represent a unique cohort for convalescent serum donation to treat the new coronavirus.
Investigators: Dr. Claudia Morris
IN PROGRESS
Emory researchers are partnering with the Georgia Department of Public Health and the Fulton County Board of Health to assist with their COVID-19-related surveillance efforts. Faculty's contributions include: geospatial analysis, patients under investigation analysis, syndrome surveillance, inequities and underlying conditions, injury, transmission dynamics, HIV, and applied mapping and spatial epidemiology.
Investigators: Drs. Uriel Kitron, Michael Kramer, Hannah Cooper, Allison Chamberlain, Neel Gandhi and Sarita Shah, and other faculty at the Rollins School of Public Health
IN PROGRESS
Researchers are working with the Water and Science Technology Board of the National Academies of Science on the use of sewage surveillance for early detection of the new coronavirus as well as strategies to safely open buildings which have been vacant for extended periods to avoid other potential contagions such as Legionnaires' disease.
Investigators: Dr. Ruth Berkelman
IN PROGRESS
Using a variety of methods, researchers will study the effects of SARS-CoV-2 infection among people living with HIV in the Atlanta area. Sites of study will include Emory and Grady hospitals, the Ponce Center, and the VA.
Investigators: Drs. Lisa Flowers, Vincent Marconi
IN PROGRESS
What is the toll of domestic violence during this pandemic? Experts are deeply concerned that workplace closures and restrictions on movement are leading to an increase in intimate partner violence. Emory researchers will interview survivors and health care providers. They will review cases and analyze trends of women seeking emergency room care at Grady Memorial Hospital in Atlanta as a result of intimate partner violence. With sufficient support, the project will also analyze domestic violence call center data. This project will reveal the specific effects of COVID-19, informing public policies and resources to prevent such violence and trauma.
Investigators: Dr. Dabney EvansIN PROGRESS
The acute and long-term effects of COVID-19 infection on brain function are not yet known. However, it can affect sensory processing, and it is known that the virus can enter the brain. This study will assess the sensory, psychomotor and cognitive abilities of patients who have recovered from COVID-19 as well as demographically matched controls who have not had the infection. The study will follow subjects at regular intervals over a year.
Investigators: Dr. Erica Duncan
IN PROGRESS
Emerging evidence suggests that SARS-CoV-2 infects the gastrointestinal tract in addition to the respiratory system. A comprehensive understanding of the gastrointestinal manifestations of this disease may have important implications in the care of affected patients and inform public health initiatives for the new coronavirus. The study will develop a registry of affected patients at medical centers nationwide and compile data on gastrointestinal and hepatological symptoms in hospitalized COVID-19 patients.
Investigator: Dr. Ambreen Merchant
IN PROGRESS
Researchers are partnering with the University of Kentucky on a project in rural Kentucky to assess the impact of COVID-19 on the re-entry experience of people who use drugs that are being released from jail.
Investigators: Dr. Hannah Cooper
IN PROGRESS
Researchers, in partnership with Children's Healthcare of Atlanta, Johns Hopkins, and Molecular Testing Labs, are conducting a survey aimed at tracking the behavioral and psychosocial impacts of the pandemic on U.S. men who have sex with men (MSM).
Investigators: Dr. Travis Sanchez
IN PROGRESS
Cancer patients who develop a COVID-19 infection have three to four times higher mortality than non-cancer patients. On the public health front, Emory researchers have partnered with the American Cancer Society to examine the association between county-level COVID-19 fatality rates and health care capacity, and to assess the impact during surges in cases. The investigators plan to regularly disseminate projections of counties with the greatest health care capacity limitations and risk of cancer treatment delays with local and national policy makers, cancer care organizations, providers, researchers, advocates, and patients.
On the clinical front, Emory oncologists are developing novel treatment approaches to improve the outcomes of cancer patients with the new coronavirus. A clinical trial is being initiated for an immunosuppressive drug to ascertain its efficacy among hospitalized patients.
Investigators: Dr. Donghai Liang (Emory Rollins School of Public Health; Dr. Ajay Nooka (Emory Winship Cancer Institute)
IN PROGRESS
Researchers are collaborating with colleagues at Harvard to study the impact of environmental factors including air pollution, temperature, and humidity on COVID-19 mortality in the United States.
Investigators: Dr. Donghai Liang
IN PROGRESS
COVID-19 is likely to present special risks to people in jails and prisons. Public health researchers are advising corrections systems on public health measures to help mitigate the spread of the virus among incarcerated people and staff. Half of people who are incarcerated have a chronic medical condition, and the incarcerated population has been graying thanks to spillover from the “three-strikes” law.
Investigators: Dr. Anne Spaulding
IN PROGRESS
Researchers are establishing a cohort of women who were infected with COVID-19 during pregnancy to measure specific blood biomarkers in these women, and then plan to establish a cohort of the offspring to examine neuropsychological development. Several new studies suggest there is an increased rate of preterm delivery and low birth weight among children born to women infected with this virus. Yet, there are major gaps in the literature. Emory researchers plan to address this need by analyzing pro-inflammatory and anti-inflammatory cytokines, as well as growth factors and indicators of fetal brain development in plasma from acute and convalescent women who were infected with COVID-19 compared to uninfected women.
Investigators: Dr. Brad Pearce
IN PROGRESS
Another Rollins team is partnering with Healthy Mothers, Healthy Babies of Georgia—a health services and advocacy organization—to gauge the perinatal health experiences of pregnant and post-partum women during the pandemic. They are collecting data to understand the psychological and health care effects of COVID-19, including the ability to seek maternity care services. This study will provide important baseline information about how to strengthen services in Georgia, which has the highest maternal mortality rate in the United States.
Investigators: Emory Rollins School of Public Health
IN PROGRESS
The School of Nursing established a Dean's Pilot Award for COVID-19 research projects and will soon award grants for two research projects, one that will focus on educational technology. Studies that nursing faculty are currently undertaking include topics ranging from the effects on cancer care, symptoms and quality of life in an autoimmune population (lupus), COVID-19 in correctional institutions, pandemic effects on the mental health of nurses, navigating healthcare by family caregivers of elders during a pandemic, COVID-19 impact on HIV care, and health disparities.
Investigators: Emory's Nell Hodgson Woodruff School of Nursing researchers
IN PROGRESS
Researchers have begun an ancillary study on stress and fear during the pandemic among vulnerable populations in Atlanta. The focus is on black adults with more than one chronic condition and their concerns. The ancillary study will inform how the pandemic changed symptoms and stress perceptions.
Investigators: Emory's Nell Hodgson Woodruff School of Nursing researchers
IN PROGRESS
The Child Health and Mortality Prevention Surveillance (CHAMPS) project, an Emory-led initiative funded by the Bill & Melinda Gates Foundation, is adjusting its efforts at sites in Africa and southeast Asia to help support COVID-19 response efforts. The project provides actionable intelligence for reducing child mortality around the world and enables the development of more effective interventions.
Investigators: Emory Rollins School of Public Health, Emory Global Health Institute
TO BEGIN
Researchers are exploring a national, collaborative longitudinal project to follow the children of pregnant women who tested positive for COVID-19. There is evidence from previous viral exposures, including the 1918 pandemic, that children born to women who have been exposed have increased risk for certain neurological issues such as schizophrenia. The investigators hope to use this study to follow an at-risk cohort to try to understand the developmental trajectory of the schizophrenia.
Investigator: Dr. David Goldsmith
TO BEGIN
Longer-term research is needed to understand the impact of COVID-19 on health care providers, nursing staff, and clinical delivery, as well as preparedness.
Investigators: Emory Schools of Public Health and Nursing
LAUNCHED
Emory public health practitioners are assisting the Africa CDC to conduct weekly COVID-19 webinars to train African clinicians about the disease and help reduce its spread in the continent.
Investigators: Dr. Scott McNabb
IN PROGRESS
The COVID-19 pandemic created an extensive need to adjust care models for patients for reasons such as limited personal protective equipment (PPE) and the need for social distancing to minimize viral spread. Emory had already implemented some aspects of telemedicine earlier including an eICU but the pandemic demanded an expansion of telehealth services. Over the last few months, Emory has invested more and more in secured telemedicine platforms, enabling health assessments to be conducted remotely via virtual- and tele-visits, resulting in telehealth services rising dramatically at Emory. The increase has allowed patients to continue to receive quality health care while safely quarantining in their homes. The expansion of telemedicine has been especially useful in treating the elderly and those in rural areas of the state. Before services could grow, significant groundwork had to be laid including developing a system-wide policy, updating access privileges, credentialing and certification for providers and staff, providing education for the appropriate practice of telemedicine while adhering to state regulations, and developing a workflow for multiple use cases. Efforts to broaden and deepen telemedicine will be ongoing.
Investigators: Dr. Greg Esper
LAUNCHED
In response to the pandemic, an advanced practice provider (APP) leadership team at Emory Healthcare redeployed its members and created alternative care models, leveraging skills sets to meet the demands in shifting areas of patient care. The skillsets of more than 1000 APPs, who comprise nurse practitioners and physician assistants, were swiftly catalogued, with leaders working with their APP teams to identify prior clinical experiences and competencies that could be used quickly to meet identified clinical needs across the organization in various areas. One of the key strategies was to provide support and relief for primary care providers for potential redeployment to areas where patients would need more care. The innovations from the APP teams in partnership and collaboration with physician colleagues minimized viral exposure to patients and staff and provided flexibility in managing services. The APP leadership team will continue to monitor and collect data, examining clinical outcomes, cost avoidance, and APP engagement, as the crisis advances in our healthcare setting. A paper on these initiatives will soon be published in Nursing Economics.
Investigators: Bonnie Proulx
LAUNCHED
During the pandemic an interprofessional team at Emory University Hospital, was tasked with identifying a process to reduce workflow burden and preserve personal protective equipment (PPE) in acute care COVID-19 units. The team developed a warm zone model (WZM) that facilitated the movement of staff between rooms of patients confirmed COVID-19 positive while wearing the same mask, eye protection, and gown. Staff were trained on extended PPE use and how to properly change gloves and complete hand hygiene between rooms of patients. The WZM reduced the overall number of PPE donning and doffing per shift, while maintaining or increasing the number of patient room entries and exits. The risk for self-contamination while doffing is well documented. Daily gown use decreased on WZM units, helping to preserve and extend current PPE supplies. Once the WZM proved successful in acute care, it was modified and instituted in critical care COVID-19 units. A paper documenting the impact of the warm zone model and how it eased workflow burden and improved teamwork while maintaining personal safety has been submitted to the American Journal of Nursing.
Investigators: Sarah Omess
IN PROGRESS
Emory's renal division has created a central database to track all COVID-19 inpatient admissions for various research activities including a national, multi-center study on acute kidney injury in the intensive care unit. Researchers at Emory Transplant Center will use the data for a local study and Emory Dialysis (outpatient clinics) is looking at effectiveness of measures to prevent spread of the new coronavirus in dialysis clinics.
Investigator: Drs. Harold Franch, Michael Connor Jr., Arpita Basu, Ibironke Apata
IN PROGRESS
Kathy Kinlaw has been leading conversation among ethics committee chairs and other key leaders across the Healthcare Ethics Consortium (HEC) during this pandemic. The HEC, which Kinlaw directs, is the main source of ethics training for hospital and health systems across Georgia and neighboring states. The goal of these discussions is to share information and resources. The HEC recently also created an ethics web resource dedicated to COVID-19.
Investigators: Prof. Kathy Kinlaw
IN PROGRESS
Researchers are analyzing national pandemic ethics policies to compile a comprehensive report that could inform best practices and guidelines for the future.
Investigators: Dr. Paul Wolpe
IN PROGRESS
Investigators have begun to look at narratives written by freshmen college students about their experiences of the COVID-19 pandemic. The longitudinal study will follow members of the class of 2023 for a year or more to track their psychological well-being and academic performance. The goal of the study is three-fold: Determine whether the self-narratives can predict better outcomes for the students; gather data for interventions that may be needed for students who are struggling; and help students have more rewarding and successful academic experiences. The student participants are drawn from Emory and four other universities across the country.
Investigators: Dr. Robyn Fivush