News Release: Research, School of Medicine, School of Public Health, Yerkes
Jan. 23, 2009
STDs Disrupt Genetic Bottleneck That Usually Constrains HIV Infection
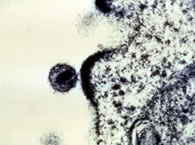 HIV "budding" out of T-cell. courtesy, Dr. Tom Folks, National Institute of Allergy and Infectious Diseases
HIV "budding" out of T-cell. courtesy, Dr. Tom Folks, National Institute of Allergy and Infectious Diseases One of the greatest challenges in fighting HIV is how fast it mutates. A chronically infected individual usually has a vast library of different viruses that could vary in their sensitivity to drugs or vaccines.
Scientists have shown that HIV faces a genetic "bottleneck" when the virus is transmitted from one person to another. It appears that most of the time during heterosexual transmission, only one virus or virus-infected cell makes it through the bottleneck to establish the new infection.
By precise genetic analysis, a team of researchers at Emory University found that the bottleneck is enlarged when the at-risk partner has an inflammatory genital infection. The infection, by disrupting normally protective mucosal barriers, allows multiple viral varieties through the bottleneck.
The results, published in the January issue of the journal Public Library of Science Pathogens, explain why other sexually-transmitted diseases make individuals more susceptible to HIV infection.
They also identify a window of time when a still-elusive HIV vaccine could control the virus, says team leader Eric Hunter, PhD, professor of pathology and laboratory medicine at Emory University School of Medicine, Emory Vaccine Center, and Yerkes National Primate Research Center.
"Very early on after initial infection, the virus is almost homogenous," he says. "It gives some hope that if the immune system can contain the virus, there might be a better chance to eliminate it. The more we know about the early stages of infection, the more likely it is we could identify ways to intervene at that critical time."
The Emory team collaborated with public health programs directed by Susan Allen, PhD, professor of global health at Emory’s Rollins School of Public Health, that enroll heterosexual couples with one HIV-positive partner in Rwanda and Zambia. These programs track more than 1,000 couples in each country and provide them counseling and condom supplies every three months. Despite these measures, a low level of HIV transmission still occurs.
"This is a unique situation, allowing us to know who transmitted to whom and compare the virus that gets transmitted to the population in the chronically infected partner," Hunter says.
The researchers identified 20 couples soon after infection occurred and obtained viral genetic sequences from both partners. They examined the most variable region of the virus’ env gene, which encodes a protein forming the outer coat of the virus.
In 18 out of 20 cases, a single viral variant from the transmitting partner initiated infection. However, that variant was not the same in each case.
"There is no single sequence that helps the virus establish itself,” Hunter says. “It just illustrates the low probability that any one variant will succeed."
The Emory team’s analysis of the 20 couples contrasts with previous studies of HIV sequences from newly infected sex workers in Kenya and sexually transmitted disease clinic patients in North Carolina, who showed more viral diversity.
For comparison with these groups, where sexually transmitted diseases are common, the Emory team analyzed a group of newly infected individuals who were infected by someone other than their spouse. This group showed more variety in viral sequences, with three out of seven individuals infected by multiple variants. Overall, out of 42 newly infected people studied to date, all five infected by multiple viral variants had evidence of genital inflammation or ulceration.
"This suggests that there is a strong barrier at the mucosal surface, which is broken down by inflammation," Hunter says. "It provides one explanation for how other sexually transmitted diseases increase the likelihood of HIV infection."
The first author is postdoctoral fellow Richard Haaland, PhD.
The research was funded by grants from the National Institutes of Health, the Bill & Melinda Gates Foundation Grand Challenges Program and the International AIDS Vaccine Initiative.
Reference:
Haaland, R.E. et al. Inflammatory genital infections mitigate a severe genetic bottleneck in heterosexual transmission of subtype A and C HIV-1 PLOS Pathogens, Vol 5, Issue 1, Jan. 2009
###
The Robert W. Woodruff Health Sciences Center of Emory University is an academic health science and service center focused on missions of teaching, research, health care and public service. Its components include schools of medicine, nursing, and public health; Yerkes National Primate Research Center; the Emory Winship Cancer Institute; and Emory Healthcare, the largest, most comprehensive health system in Georgia. The Woodruff Health Sciences Center has a $2.3 billion budget, 17,000 employees, 2,300 full-time and 1,900 affiliated faculty, 4,300 students and trainees, and a $4.9 billion economic impact on metro Atlanta.
Learn more about Emory’s health sciences:
Blog: http://emoryhealthblog.com
Twitter: @emoryhealthsci
Web: http://emoryhealthsciences.org
