Living (with cancer)
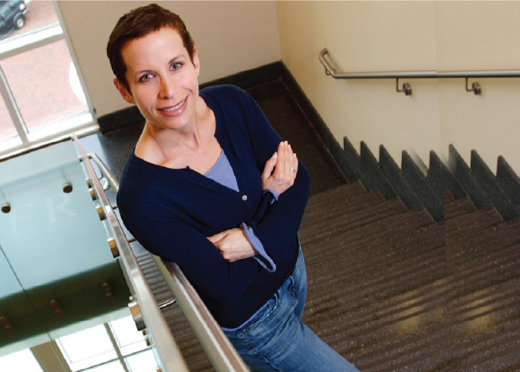
Kristen Moss was enrolled in a clinical study at Winship Cancer Institute.
by Martha Nolan McKenzie
|
|
A few weeks before she was scheduled to have her first mammogram, Kristen Moss discovered a lump in her breast.
A biopsy confirmed that the lump was cancer—specifically, HER2 positive breast cancer, a typically aggressive form. When Moss, 40, asked a friend at the American Cancer Society where she should go for treatment, the friend sent her to Emory Winship Cancer Institute.
At Winship, Moss was enrolled right away in a clinical study testing a novel combination of chemotherapy drugs formulated for her specific type of tumor. After only eight weeks of treatment, an MRI showed no signs of the cancer. She finished the 20-week chemo regimen in October, followed by a mastectomy and reconstructive surgery.
"If I had to have breast cancer, I'm glad I have it now when so many advances have been made, and I'm glad I can be treated at Emory," says Moss. Just a few years ago, Moss would have had to go out of state to find this kind of treatment. However, in those years, both Emory and Georgia have been pouring massive resources into Winship to build a world-class, matrix cancer center (see box below). The institute offers patients a breadth and depth of cancer care from basic science research and clinical trials to prevention in the larger population.
"Matrix cancer centers are engines for scientific discovery," says Winship's director Brian Leyland-Jones. "Most significant advances in cancer research and care are developed at academic cancer centers."
Emory hopes to parlay strengths—including leadership in basic science, surgical oncology, nanotechnology, health disparities research, and imaging technologies—into designation by the National Cancer Institute (NCI) as a comprehensive cancer center. The designation would bring more NCI funding and clinical trials to Winship—and to Georgia. And that translates into more help and hope for Georgians with cancer.
It was this goal that prompted the state, through the Georgia Cancer Coalition (GCC), to invest $50 million from tobacco settlement funds in Winship. "We are the largest state in the nation without a comprehensive cancer center," says William Todd, GCC president and CEO. "It goes way beyond window dressing or civic boasting. In our quest to shorten the time from discovery to application, we need robust clinical trial networks where investigator-initiated trials at an NCI center are available to community hospitals, bringing the benefits of science to patients more quickly. A comprehensive cancer center designation for Winship would bring more of those NCI clinical trials to Georgia."
From the bench
In the beginning, there is a gene that mutates. That's the genesis of every cancer. Trying to identify those genes, determining what causes them to mutate, and developing agents that can either prevent or repair the damage or stop the defective cells from multiplying is a major focus of Winship's basic scientists.
In one approach, researchers there are studying the ability of tumor cells to repair damage to their DNA caused by an anti-tumor treatment. "That's why you can kill 99% of a tumor cell population and not wipe out the cancer," says Paul Doetsch, Winship's deputy director for basic research. "That remaining 1% evolves into a drug-resistant form and then grows. So if we are able to target the tumor's DNA repair pathway with a drug, in many cases we could eliminate the tumor cells' ability to become resistant, thus making them sensitive to treatment."
That's what Winship investigators are trying to do with triple-negative breast cancer. The most aggressive form of breast cancer, it strikes African-American women at twice the rate of whites. Triple-negative breast cancer is so named because it lacks three receptors known to fuel most breast cancers, and that means this type of cancer is incredibly resistant to the most successful treatments for breast cancer, which target these receptors.
A Winship team of basic science researchers has proven successful in overcoming that resistance by reactivating estrogen and progesterone receptors in triple-negative breast cancer cells in the lab. That reactivation rendered them sensitive to tamoxifen, the most widely used drug to treat breast cancer.
The basic scientists then handed off the lab results to a clinical team, which is using them to design a clinical trial to be conducted with seven community hospital partners throughout the state. "This work could not have been done at any place other than a matrix cancer center," says Doetsch. "At Emory, our basic science information gets translated into animal studies or cell culture studies, which are then used to inform clinical trials that may have a very real positive impact on patients."
To patients
Translating research into practice is the ultimate goal of the cancer center. Discoveries in the lab are used to develop new drugs and therapies, which may then be tested in clinical trials. The trip from the research bench to the bedside is often a relatively short one at Winship, just as it was for Kristen Moss.
One reason for that is Emory's support of interdisciplinary collaboration, says Fadlo Khuri, chair of of hematology and medical oncology at Emory and deputy director for translational research at Winship. "Because of the complexity of the many diseases known as 'cancer,' finding new avenues for prevention, causes, treatments, and cures involves work in a host of scientific disciplines from chemistry and epidemiology to pathology and oncology. These disciplines and others all come together within Winship."
In fact, Emory has one of the strongest collaborative environments of any institution on the country, says Dong Moon Shin, director of Winship's chemo-prevention program. "At other institutions, researchers compete for tumor tissue, for access to imaging, for resources, but here everyone is on the same team. As a result, discoveries in the lab tend to get translated into treatments more quickly."
A group of Emory researchers, for example, has developed a biodegradable nanodrug that promises to attack cancer cells while leaving healthy cells untouched. The team created a nanoparticle by linking the cancer drug Taxol and folic acid with a biodegradable heparin molecule. The folic acid acts like a heat-seeking missile, flying past normal cells to crash into the many folate receptors in head and neck tumors to deliver its payload of Taxol. Since normal cells are unaffected, the often debilitating side-effects of chemo are avoided. The nanodrug showed promising results in animal studies, and Shin hopes to follow up with a clinical trial soon.
Other new drugs and therapies have already moved to the next step. One of those is testing the effectiveness of a drug combo–growth factor inhibitor EGFR-TK1 and anti-inflammatory celecoxib—in blocking the formation of tumors in pre-malignant cells. Participants in the trial are typically current or past smokers who have pre-malignant cells in their mouth or throat. "We know this is a very high-risk population, and untreated, about half of these people will develop cancer," says Shin.
In pre-clinical studies, this drug combo not only has blocked the development of pre-malignant cells into cancer cells but also has caused cells to revert back to their normal, healthy state. Shin's team is running a trial to see if the same drug combo can prevent degradable heparin molecule. The folic acid acts like a heat-seeking missile, flying past normal cells to crash into the many folate receptors in head and neck tumors to deliver its payload of Taxol. Since normal cells are unaffected, the often debilitating side-effects of chemo are avoided. The nanodrug showed promising results in animal studies, and Shin hopes to follow up with a clinical trial soon.
Other new drugs and therapies have already moved to the next step. One of those is testing the effectiveness of a drug combo–growth factor inhibitor EGFR-TK1 and anti-inflammatory celecoxib—in blocking the formation of tumors in pre-malignant cells. Participants in the trial are typically current or past smokers who have pre-malignant cells in their mouth or throat. "We know this is a very high-risk population, and untreated, about half of these people will develop cancer," says Shin.
In pre-clinical studies, this drug combo not only has blocked the development of pre-malignant cells into cancer cells but also has caused cells to revert back to their normal, healthy state. Shin's team is running a trial to see if the same drug combo can prevent recurrence of cancer in those who have already been treated successfully for head and neck cancer.
For patients, the ability to enroll in a clinical trial is a godsend. "I believe the best care for any patient is through participation in high-quality clinical trials," says Walter Curran, Winship's chief medical officer. "That's where they'll receive the most advanced, cutting-edge treatments. And the more trials a center has available, the greater the likelihood that the patient will have an opportunity to participate."
Winship patients are getting more and more of these opportunities, thanks in part to Curran. For the past decade, he has served as national group chair of the Radiation Therapy Oncology Group (RTOG), the world's leading research group conducting major multicenter clinical trials for radiation therapy for cancer. When Curran joined Winship in 2008, he brought the RTOG trials with him.
In addition, Emory's work in the community is increasing awareness about cancer prevention, screening, and access to care. A recent study by Emory researchers at the AVON Comprehensive Breast Center at Grady Memorial Hospital found that community-based programs aimed at raising awareness and use of breast cancer screening may improve breast cancer survival rates for African-American women, who have a higher risk of death from the disease.
And beyond
Promising new cancer drugs and clinical trials may capture the most news headlines, but prevention is given equal weight at Winship. "Prevention really goes to the heart of the matter," says Theresa Gillespie, Winship's deputy director for administration. "We want to be able to predict who might get cancer so we can intervene or encourage them to engage in activities to prevent cancer from the get-go."
Winship epidemiologists, behavioral scientists, and health policy experts are teaming up to understand how lifestyle and diet influence a person's risk for developing cancer. They are developing biomarkers to determine who is at elevated risk for certain types of cancers. They are deciphering how societal forces (such as insurance, access to health care, and economics) impact cancer outcomes. And they are finding ways to prevent co-morbidities or additional disorders such as depression and sleep problems in patients who have cancer.
Toward those ends, Winship, in collaboration with the GCC, is mounting an aggressive study that will identify 140,000 cancer-free subjects throughout Georgia and follow them for decades to see who develops cancer and who doesn't.
"For each subject, we'll collect a wealth of personal and medical history information via questionnaires. We'll collect blood and urine samples and store them," says epidemiologist Robin Bostick, leader of the Cancer Control and Population Sciences project. "We'll check in with them every year or two. Then, when enough people have developed a certain type of cancer, we will do analyses to see the differences between the people who developed it and those who didn't. Did they tend to exercise less? Smoke more? Eat more animal fat?"
The potential impact of the Georgia Cancer Cohort Study is immense. "It aims to do for cancer what the Framingham Heart Study has done for cardiovascular disease," says GCC's Todd, referring to the 50-year landmark heart study of residents of Framingham, Mass. "It was from the Framingham study that the concept of risk factors first emerged. As a result, the incidence of heart disease in this country has been decreasing for the past 35 years. We hope to identify similar risk factors for cancer and eventually see a fall in its incidence."
The Georgia cohort study offers researchers a particularly wide window on cancer because of the diversity of the state's population. "There are other prospective cohort studies, but they tend not to be representative of the general population," says Bostick. "In Georgia, we have a diverse population —racially, ethnically, and in terms of rural versus urban. This will help us identify disparities in the incidence of cancer."
For her part, Moss was unaware of the research and translational clinical trials going on at Winship. She just knew she was getting the best cancer care possible, and she was getting it at home. And that's all that mattered.
|
|
Diagnosing without drillingBrain tumor biology is hard to ferret out because of the tumor's location inside the skill, a particularly difficult place to access. "With imaging, you don't learn very much," says Irwin Van Meir, co-director of Winship's brain tumor working group and director of the lab for molecular neuro-oncology. "You might be able to detect that something is there, but it doesn't tell you much about the biology of the tumor." So Van Meir and his colleagues began looking for clues in a different place—in the cerebral spinal fluid (CSF) that surrounds the brain and the spinal column. It was, it turns out, a good place. Proteins secreted by brain tumors end up in the CSF. Working with scientists in the core facilities that support biomarker research, Van Meir imbedded nanoparticles—tiny magnetic particles—with scores of different antibodies, each attracted to a different specific protein, and introduced the particles into CSF drawn from brain tumor patients. The result: the scientists not only identified more than 100 proteins in the CSF but also developed a signature of proteins that could determine specifically what type of brain tumor was present. "A spinal tap is a little more invasive than a blood draw, but it is nothing in comparison to having someone drill a hole in your head," says Van Meir. "Potentially you could combine nanoparticles with your favorite 'sticky glue,' such as antibodies that hone in on something very specific, then inject them into the patient. If a tumor is present, the antibodies will cover it, and the nanoparticles, since they are magnetic, will show up on an MRI. So potentially you'll not only be able to see if a tumor is there, but depending on which antibodies were attracted to it, exactly what type of tumor it is." Emory's brain tumor program also is participating in the Cancer Genome Atlas, an NIH project that will catalogue DNA alterations in brain, lung, and ovarian cancers with the goal of finding new treatments. |




