A hybrid treatment for cancer
Field Willingham is working to halt the progress of esophageal conditions before they become malignant, using therapies that are minimally invasive. |
Patients who are diagnosed with esophageal cancer face a daunting prognosis: pain, fatigue, weakness, and difficulty eating.
In some advanced cases, all or part of the esophagus and stomach may have to be removed.
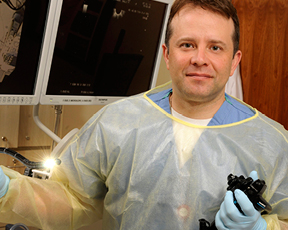
But early detection and a new approach to treat esophageal lesions promises to ease the burden and may offer a more hopeful prognosis for esophageal cancer. Emory gastroenterologist Field Willingham and his colleagues are using several minimally invasive therapies to treat lesions and have developed a new hybrid approach to treat tumors in the upper GI tract.
The flow of stomach acid into the esophagus can lead to gastroesophageal reflux disease (GERD), which in turn can lead to a condition known as Barrett’s esophagus. Barrett’s esophagus occurs when the cells in the lower esophagus begin to look more like cells from the intestine. Over years, Barrett’s esophagus can become low-grade dysplasia, then high-grade dysplasia, and even maybe esophageal cancer.
“We are trying to intervene when the disease is at a premalignant stage, before the Barrett’s has progressed to cancer,” Willingham says. “If we can catch the Barrett’s in the premalignant stage, we can use an endoscopic approach to treat just the lining layer of the esophagus.”
In many cases, the team can get rid of the bad cells in a short endoscopic procedure. Endoscopy involves passing a slender, tube-like instrument into the esophagus to treat just the lining layer. Often the approach can keep patients from progressing to a more severe stage and spares them a radical esophagectomy.
Among the endoscopic techniques in the surgeons’ toolbox is an endoscopic mucosal resection (EMR), during which they apply a band around the area that contains the troublesome cells. The band raises the tissue into a polyp of sorts, allowing them to remove the polyp and take the bad cells while leaving the deeper esophagus intact. The lining grows back normally, allowing some patients to avoid the debilitating side effects of major surgery.
After EMR, Willingham and his team use other techniques to get rid of the premalignant cells (radiofrequency ablation, which uses a balloon or small pad to apply energy to the lining layer of the esophagus, and cryotherapy, which freezes just the bad cells in the lining layer with liquid nitrogen). Almost all patients go home the same day, and only a few have any discomfort.
For more advanced tumors, teams from surgery and gastroenterology use thin laparoscopic instruments and flexible endoscopes to remove larger tumors that previously would have required major surgery. Working together, they have been able to spare five of seven recent patients a major life-altering surgical resection.
Detecting and removing esophageal tumors early is essential for a favorable outcome. Once tumors progress, the prognosis can be grim and morbidity high. The hope is to offer all patients an excellent outcome with the least invasive approach. —Robin Tricoles
|
Web Connection: To learn more about treatments for esophageal cancer, call 404-778-7777 or visit emoryhealthcare.org/connecting/healthconnection.html. |


