







|
 |
 |
Big
problems, big science, better health
The stress of battle
40 life-changing minutes
Progesterone and traumatic brain injury
New synergy in cancer
|
Tracking
brain tumor treatment
Noteworth
Built
from scratch
High marks from NIH
A
new formula for matching kidneys |
 |
 |
 E-mail
to a Friend
E-mail
to a Friend  Printer friendly
Printer friendly |
 |
|
|
|
 |
Big
problems, big science, better health
The numbers are sobering. A third of the world's 40 million
people with HIV/AIDS are also infected with TB. Of those, 90%
die within months of contracting TB if they are not treated properly.
Finding effective treatments is growing more difficult as various
strains of TB are becoming more widespread and more virulent,
especially in sub-Saharan Africa and India.
Researchers at Emory and in India
are determined to find a solution. Emory's Global Health
Institute, the Emory Vaccine Center, and the International Center
for Genetic Engineering and Biotechnology (ICGEB) have created
the Center for Global Vaccines, based at the ICGEB in New Delhi.
"Our initial studies will
focus on the basic aspects of HIV/TB co-infection," says
Rafi Ahmed, director of the Emory Vaccine Center. "In fact,
the World Health Organization has just classified HIV/TB as a
unique disease."
India now has the largest number
of HIV-infected people in the world, and 5.7 million of them have
HIV/TB. Although a vaccine exists to prevent TB, it can be used
only in limited circumstances. Thus, Emory and the ICGEB will
focus on developing a therapeutic vaccine that can be used more
widely—one that can be given to people already infected
with HIV/TB. "We want to tackle very big problems, and this
is a very big problem," says Ahmed. "This is very
big science."
"Big" also describes the
new Global Health Institute, a multidisciplinary umbrella for
Emory faculty, students, and alumni who want to solve the world's
critical health problems. Led by Jeffrey Koplan, vice president
for academic health affairs and former CDC director, the institute builds on Emory's history of
global partnerships in medicine, public health, and other disciplines.
former CDC director, the institute builds on Emory's history of
global partnerships in medicine, public health, and other disciplines.
The institute represents a major
commitment by the university. Its $110 million budget includes
$55 million from the university and $55 million from sources in
and outside of Emory.
Among the institute's new programs
is the Republic of South
Africa Drug Discovery Training Program to provide young African
scientists with experience in translating research into health
care solutions. Emory chemist Dennis Liotta, co-inventor of several
successful anti-HIV/AIDS drugs, leads the program. Reynaldo Martorell,
public health professor, directs the Partners in Global
Health Program, an expanded collaboration with the National Institute
of Public Health in Mexico.
Other global health projects will
focus on public health research and training in developing nations,
health care workforce shortages, international bioethics, and
the health impact of global migration.
A separate program affiliated with the institute is the International
Association of National Public Health Institutes, an alliance
of CDC-like agencies dedicated to optimizing global health by
improving public health infrastructure around the world. Koplan
serves as association president.
Learn
more about the Global Health Institute. |
 |
|
|
|
 |
| |
|
|
| |
The
stress of battle
|
|
| |
Despite
ongoing media coverage, it's still hard to fathom
the mental toll of the Iraq war on U.S. veterans. In a study
funded by the Department of Veterans Affairs, Emory researchers
are testing a new method for treating post-traumatic stress
disorder that may help soldiers deal with troubling memories before depression, memory loss, drug abuse, and other health
problems occur.
before depression, memory loss, drug abuse, and other health
problems occur.
The treatment, mindful based
stress reduction (MBSR), is an eight-week program that teaches
participants how to "intentionally pay attention to
present-moment experiences" such as physical sensations
or perceptions without evaluating those experiences. During
each session, participants are introduced to techniques
such as yoga and meditation. MBSR uses "teachers"
and "students" instead of "patients"
and "therapists."
"We know that medications
sometimes have unpleasant side effects or don't work
at all," says lead investigator J. Douglas Bremner,
director of mental health research at the Atlanta VA Medical
Center. "MBSR is an intervention that not only teaches
a soldier how to cope with painful memories from battle,
but can also be beneficial as a coping skill for life in
general." |
|
| |
|
|
|
 |
|
|
|
 |
| |
|
|
| |
40
life-changing minutes
|
|
| |
The
40 minutes the doctor spent with Amy changed her life. It
appeared to be a simple case: She needed the stitches in
her arm removed. But only when Sheryl Heron questioned her
about why she put her hand through a window did the truth
come out. Amy was a victim of intimate partner violence.
Heron gave her information
on resources to help her should she decide to leave her
abuser—often the time when abuse is especially violent—and
then Amy was on her way. Only a yea r
later did Heron know the extent of her influence. Amy emailed
her that she had left the relationship, moved to Florida,
and re-enrolled in college. r
later did Heron know the extent of her influence. Amy emailed
her that she had left the relationship, moved to Florida,
and re-enrolled in college.
Gone are the days of patch
‘em up, move ‘em out. Emergency room doctors
and residents now know if they look beyond the injury or
complaint and find domestic violence, addressing the root
cause will help prevent future visits and thus ease the
caseload in the ER. "If you take the time on the front
end to manage what is bringing them in on the back end,
they don't come back," says Heron. "In
the end, you have to consider we are talking about human
beings and their lives."
However, most medical schools
don't have dedicated curricula on domestic violence,
be it children, intimate partner, or elderly. As the new
assistant dean for medical education and student affairs
at Grady Hospital, Heron decided a family violence workshop
was in order for M3 students. The daylong workshop last
fall featured a number of experts in and outside of Emory,
including a staff member of the Grady Rape Crisis Center;
former juvenile court judge Robin Nash, now director of
the Barton Child Law and Policy Clinic in Emory's
School of Law; and a survivor of sexual abuse. All provided
insight on their experiences.
"Medicine teaches us
to fix things," says Heron. "Laceration? Suture
it. Infection? Give an antibiotic. Domestic violence doesn't
have a magic pill, a magic solution. I try to teach physicians
it takes six or seven times for a woman to tell about violence.
We need to consider how we impact people's lives."
|
|
| |
|
|
|
 |
|
|
|
 |
Progesterone
and traumatic brain injury
Progesterone
may be key to reducing death and disability in patients with traumatic
brain injury (TBI). It also appears to be safe. Emory researchers
based these findings on the first clinical study of its type in
the world.
Prior to this study, progesterone
treatment for TBI was studied in laboratory animals for as long
as 15 years. The researchers conducting the clinical trial based
their work on the foundation laid by Emory neurobiologist Donald
Stein, who discovered the neuroprotective effects of progesterone
in the laboratory.
Patients enrolled in the double-blind
study at Grady Hospital had to reach the hospital within 11 hours
of injury. Patients in the study had a blunt traumatic injury,
typically caused by a car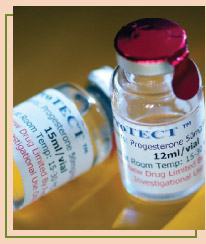 accident, motorcycle crash, or fall. Enrolled patients had an
initial Glasgow coma scale (GCS) score ranging from 4 to 12. A
score of 4 to 8 signals severe TBI, usually accompanied by coma,
while a score of 8 to 12 signals moderate TBI. Four out of every
five patients enrolled received intravenous progesterone, and
one of every five patients received a placebo. Thirty days after
injury, researchers used objective rating scales to assess each
patient's neurologic function and level of disability.
accident, motorcycle crash, or fall. Enrolled patients had an
initial Glasgow coma scale (GCS) score ranging from 4 to 12. A
score of 4 to 8 signals severe TBI, usually accompanied by coma,
while a score of 8 to 12 signals moderate TBI. Four out of every
five patients enrolled received intravenous progesterone, and
one of every five patients received a placebo. Thirty days after
injury, researchers used objective rating scales to assess each
patient's neurologic function and level of disability.
"We found encouraging evidence
that progesterone is safe in the setting of TBI, with no evidence
of side effects or serious harmful events," says David Wright,
the emergency medicine physician who led the study. "In
addition, we found a 50% reduction in the rate of death in the
progesterone-treated group. Furthermore, we found a significant
improvement in the functional outcome and level of disability
among patients with moderate brain injury."
Wright's team found no major
differences in the rate of adverse effects among patients who
received progesterone compared with those who received placebo.
About 30% of patients given placebo died within 30 days of injury,
compared with only 13% of those given progesterone. Most patients
who died had severe TBI. Because more severe TBI patients in the
progesterone group survived, it was not surprising that they had
a higher average level of disability at 30 days than survivors
in the placebo group.
Progesterone is a promising treatment
for TBI because it is inexpensive, widely available, and has a
long track record of safe use in humans to treat other diseases.
Wright's team is planning a large, multicenter Phase III
trial to test the effectiveness of progesterone in 1,000 patients
with TBI. In the future, they plan to study the effects of progesterone
treatment in animal models of blast-related injury, a major cause
of death among combat personnel. They also hope to study the use
of progesterone to treat children with brain injuries.
View
a video about the progesterone study |
 |
|
|
|
 |
| |
|
|
| |
New
synergy in cancer
|
|
| |
 Brian
Leyland-Jones is the new associate vice president and director
of the Winship Cancer Institute. Leyland-Jones, who specializes
in breast cancer, is known internationally for developing
individualized therapies and novel clinical trials. He comes
to Emory from McGill University in Montreal, where he served
as the Minda de Gunzberg Chair in oncology, professor of
medicine, and director of McGill's Comprehensive Cancer
Center. Brian
Leyland-Jones is the new associate vice president and director
of the Winship Cancer Institute. Leyland-Jones, who specializes
in breast cancer, is known internationally for developing
individualized therapies and novel clinical trials. He comes
to Emory from McGill University in Montreal, where he served
as the Minda de Gunzberg Chair in oncology, professor of
medicine, and director of McGill's Comprehensive Cancer
Center.
At McGill, he led the development
of a clinical trials operation that integrated research
with five clinical trial cooperative groups and more than
40 pharmaceutical companies. His research interests include
pharmacodynamics, pharmacokinetics, and pharmacogenetics
in clinical trials; translation of preclinical models into
the clinic; biomarker endpoints in Phase I/II clinical trials;
and screening and mechanistic studies of novel targeted
and chemotherapeutic anti-cancer agents. |
|
| |
|
|
|
 |
|
|
|
 |
| |
|
|
| |
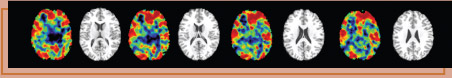
Tracking
brain tumor treatment
|
|
 |
| |
A
newly identified novel biomarker potentially could help
physicians better determine when a brain tumor spreads or
recurs after treatment, reports Winship Cancer Institute
researcher Erwin Van Meir.
The biomarker, a protein known
as "soluble attractin," is normally absent in
the central nervous system (CNS) and undetectable in cerebral
spinal fluid (CSF) unless malignant astrocytomas—the
most common form of intracranial tumors—are present
in the CNS. The CSF can be sampled for analysis of proteins
secreted by CNS tumors.
This newfound ability to identify
biomarkers for malignant astrocytomas means that physicians
will have a minimally invasive method to track the success
of treatments. These biomarkers, singly or in combination,
will provide a fingerprint of the disease and in the future
better define the disease, predict what type of treatment
to use, and allow doctors to monitor how well the tumor
responds to treatment.
"Using proteomic analysis
of the CNS of patients with brain tumors, we have identified
for the first time that attractin levels are elevated in
patients with high-grade astrocytoma," says Van Meir,
who led the study in collaboration with the Dana Farber
Cancer Institute. "Because few noninvasive methods
are available for monitoring CNS malignancies, there is
an urgent need to find reliable indicators." |
|
| |
|
|
|
 |
|
|
|
 |
Noteworthy
Michael
Johns,
who has led the Woodruff Health Sciences Center for 11 years,
will become chancellor of Emory this fall. In addition to advising
the president and the board of trustees, Johns will represent
the university on health care policy and building partnerships,
such as Emory's research collaboration with Georgia Tech.
For the first time, two
Emory health administrators hold top leadership positions with
the Association of American Medical Colleges (AAMC). Michael Johns,
CEO of the Woodruff Health Sciences Center, is immediate past
chair of the Council of Teaching Hospitals and Health Systems.
Thomas Lawley, dean of the School of Medicine, chairs the AAMC's
Council of Deans.
Physicians with Emory Healthcare provided $70.7
million in charity care in 2005–2006, a 7% increase over
the previous year. At publicly funded Grady Hospital, Emory provided
$24.7 million in uncompensated care, up $2.7 million from the
previous year. About 85% of the physicians at Grady are Emory
medical faculty. |
 |
|
|
|
| |
| |
|
|
| |
Built
from scratch
|
|
| |
Emory
University Hospital opened a neuro critical care unit that
centralizes most critical medical services for patients
suffering from severe neurologic trauma—including
severe brain injury, strokes, and aneurysms. Just as important,
the unit's design incorporates the importance of family
in the patient's healing.
One of the largest in the
United States and one of only a few of its type in the Southeast,
the unit is staffed by
neurointensivists, critical care nurses, nurse practitioners,
and pharmacists. All played a role in creating the unit,
along with social workers, former patients, and family members.
social workers, former patients, and family members.
"Plans for the neuro
ICU incorporate core principles of evidence-based, patient-centered
design—a holistic approach that focuses on the patient's
physical environment as a tool for healing," says
Owen Samuels (shown left), director of neuroscience critical
care. The unit's design takes into account factors
such as the effects of natural light, noise reduction, and
increasing staff efficiencies.
Also key is sufficient space
to perform intricate procedures at the bedside and thus
reduce transporting fragile patients across the hospital.
A high-resolution CT machine is housed in the unit, allowing
patients to be scanned upon admission and during their stay.
"This unit," says Emory Healthcare president
and CEO John Fox, "has raised the proverbial ‘bar'
and set the standard, locally and nationally, for critical
care."
Learn
more the neuro icu. |
|
| |
|
|
|
|
|
|
|
 |
| |
|
|
| |
High
marks from NIH
|
|
| |
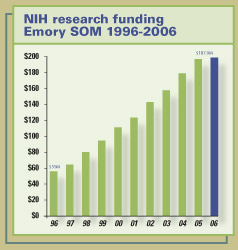
The School of Medicine now ranks 18th among all U.S. medical
schools in total research grants awarded by NIH for 2006.
The school has climbed steadily in research funding, having
ranked 31st in 1996.
|
|
| |
|
|
|
 |
|
|
|
 |
A
new formula for matching kidneys
Many patients on the national waiting list for kidney transplants
have only a small chance of receiving a new organ, no matter
how long they wait. Because of previous transplants, pregnancies,
or blood transfusions, these patients have developed antibodies
that make it difficult to match them with donor organs.
Emory researchers have developed the
Emory Algorithm, a decision process that may give new hope to
these highly sensitized patients. The algorithm may even change
the way kidneys from deceased donors are allocated in the United States.
deceased donors are allocated in the United States.
Sensitized patients have developed
antibodies against human leukocyte antigens (HLAs), which play
an important role in the body's immune response to foreign
tissue. While these patients represent one-third of the national
waiting list for kidney transplant patients (and 50% in Georgia),
they receive about 15% of deceased-donor kidney transplants
each year.
The United Network for Organ Sharing
coordinates the nation's transplant system through a point
system primarily based on wait time, sensitization, and HLA
matching. When a "perfect match" occurs, the kidney
is offered to the person at the top of the national list. If there are no perfect matches, the kidney becomes
available to transplant centers in the region from which it
came.
national list. If there are no perfect matches, the kidney becomes
available to transplant centers in the region from which it
came.
The Emory Algorithm follows these
guidelines but also allows a transplant center to predict which
sensitized patients on the list will be compatible with any
given donor. A five-year study, published in the American
Journal of Transplantation, found the algorithm raised
the kidney transplant rate from 15% to 25% by accurately predicting
which sensitized patients would be compatible with the donor
kidney. In the study, the survival rate for sensitized patients
was almost identical to that of unsensitized recipients—66%
versus 70%.
Immunologists Robert Bray and
Howard Gebel, along with transplant surgeons Christian Larsen
and Thomas Pearson, developed the algorithm. They used a relatively
new technology of single-antigen bead assays. This method analyzes
HLA antibodies more specifically by identifying a single antibody
at a time versus general groups of antibodies. The algorithm
allows immunologists to inform transplant surgeons with a high
degree of confidence whether a kidney from a deceased donor
is a compatible match with a recipient. |
 |
| |
|
|
| |
|
|
|
|
|





