 |
| |  | Vikas P. Sukhatme, MD, ScD |
As we begin 2018, I want to express my sincere thanks to all of you for welcoming me so warmly to the Emory School of Medicine. It has been a pleasure meeting many of you in person over the past several weeks. During the faculty town hall meeting on December 19, I mentioned how much I value my three-o-clock adventures, when I leave my fourth-floor office in the SOM with the intention of simply visiting with, being inspired by, and learning from our amazing students, faculty and staff.
If you did not attend the town hall, I hope you will take a few moments to view this video. I came to Emory because, simply put, what we do here can change the world. I believe this is a unique time in Emory history. From the expansive knowledge base and talent of our faculty and staff, to the infusion of energy and fresh ideas from our leaders, to the ability to accelerate progress through ongoing developments in technology, we have the opportunity to provide innovative answers to even the boldest questions. I hope you'll join me. | Town Hall Video | |
| |
|  | | Standard guidelines for stroke treatment currently recommend clot removal only within six hours of stroke onset. But a milestone study with results published in the New England Journal of Medicine shows that clot removal up to 24 hours after stroke led to significantly reduced disability for properly selected patients. Raul Nogueira (neurology, neurosurgery, radiology) served as co-principal investigator, along with Tudor Jovin at the University of Pittsburgh.
The international multi-center clinical study, known as the DAWN trial, randomly assigned 206 stroke victims who arrived at the hospital within six to 24 hours to thrombectomy, or to standard medical therapy. Almost half of the patients (48.6 percent) who had clot removal showed a considerable decrease in disability, meaning they were independent in activities of daily living 90 days after treatment. Only 13.1 percent of the medication group had a similar decrease. There was no difference in mortality or other safety end-points between the two groups.
To select patients for the trial, the researchers used brain imaging and clinical criteria as opposed to just time alone. "Looking at the physiological state of the brain and evaluating the extent of tissue damage and other clinical factors seems to be a better way to decide if thrombectomy will benefit patients as opposed to adhering to a rigid time window," said Nogueira. The researchers planned to enroll a maximum of 500 patients. However, a pre-planned interim review of treatment effectiveness led the independent Data Safety Monitoring Board to recommend early termination of the trial, based on criteria demonstrating that clot removal provided significant clinical benefit in the studied patients.
Grady was the second leading site for DAWN trial enrollment, which included sites in the United States, Spain, France, Australia and Canada. | Learn More | |
| |
| | Tammie Quest (emergency medicine) has been recognized by her peers in the American Academy of Hospice and Palliative Medicine as one of the 30 most influential leaders in the specialty. Quest is a nationally recognized expert in palliative care in the emergency setting and has a lifelong dedication to integrating emergency medicine and hospice and palliative medicine.
"This is a tremendous honor to be recognized by our field," Quest says. "I have always let my passion to improve the patient and family experience of serious illness guide my work in all settings. I was born and raised as an emergency physician dedicated to helping those most in need. This was and is inspirational to my life's work, as I remain drawn deeply to the calling to relieve pain and suffering of those with serious illness and end of life needs. While we often call it work, I am fortunate that I have never really worked a day in my life. When you live your life's passion to help make our field better, you are not working, you are just living and giving. That's where I always want to be." | Learn More | |
| |
| 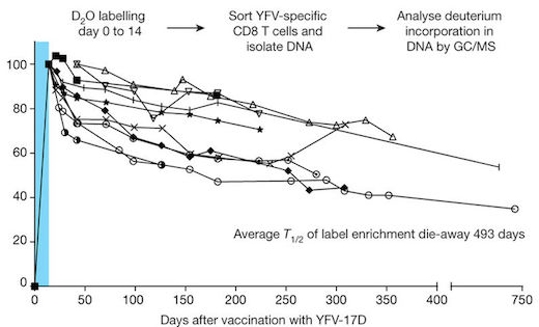 | | Memory T cells earn their name by embodying the memory of the immune system – they help the body remember what infections or vaccines someone has been exposed to. But to become memory T cells, the cells go backward in time, relinquishing their status as immune foot soldiers.
This is a key finding of two Nature papers, published on December 13. Their results inform a debate among immunologists about memory T cell development, with potential implications for vaccine design.
Memory CD8 T cells are trained to kill cells that may have been infected by a virus or display a sign of not belonging. What distinguishes memory CD8 T cells from untrained naïve cells is that they can respond rapidly, within minutes or hours. The new research illuminates how the memory cells accomplish this – their genes are poised to respond, even years after initial activation, says Rafi Ahmed (microbiology, immunology), senior author of both papers. | Learn more | |
| |
|  | | (Row 1, L to R) Jonathan Langberg, Barbara Rothbaum, Jonathan Ho-Youn Kim, and Pratik Sandesara. (Row 2, L to R) Michael Burke, Marilane Bond, Marcus Urquiaga, and Amy Dryman | Notables | Jonathan Langberg (cardiology) and Barbara Rothbaum (psychiatry) were named fellows of the National Academy of Inventors, a high professional honor bestowed to academic inventors who have demonstrated a prolific spirit of innovation in creating or facilitating inventions that have made a tangible impact on quality of life, economic development and the welfare of society. Langberg is a pioneer in the development of radiofrequency ablation, and Rothbaum is an innovator in the application of virtual reality exposure therapy to the treatment of psychological disorders.
Three SOM cardiologists are recipients of the 2017 Northwestern Cardiovascular Young Investigators' Forum awards, which encourage and recognize young physician-scientists: Jonathan Ho-Youn Kim (Clinical Research, 3rd Place, Junior Faculty), Pratik Sandesara (Clinical Research, 2nd Place, Fellows) and Michael Burke (Basic Science Research, 3rd Place, Junior Faculty).
Marilane Bond (associate dean, medical education) was elected to the Board of Directors of the Accreditation Council for Continuing Medical Education (ACCME). The Council's mission is identification, development, and promotion of standards for quality continuing medical education.
Marcus Urquiaga (administrator, nephrology) and Amy Dryman (training coordinator, Division of Animal Resources) received Emory University Awards of Distinction. Since 1985, the annual award has recognized staff members who have made outstanding contributions to the Emory community. Honorees were celebrated at dinner with President Claire Sterk and received a $1,000 award. | |
| |
|
