New urgent care and MinuteClinic options |

Meet the Class of 2017 |

Working the night shift in daytime |
 In brief |
|||||
| October 26, 2016 | |||||||||
Emory research funding totals record $574.6 million for FY 2016
Emory researchers received $574.6 million from external funding agencies in fiscal year 2016, the largest total in Emory's history. This marks the seventh consecutive year that research funding has exceeded $500 million. Federal agencies awarded $389.7 million, led by the NIH, with $333 million in awards, or 85% of total federal dollars awarded to Emory. WHSC researchers received more than $540 million in FY 2016, or nearly 94% of the university total, with $364.9 million in federal funding. The schools of medicine, nursing, and public health and Yerkes all had increased funding over FY 2015 totals: - Medicine: $348 million Examples of Emory’s externally funded research projects in fiscal year 2016 include - $35.6 million to develop new strategies for preventing and curing AIDS, $8.3 million to establish a National Exposure Assessment Laboratory to measure the impact of environmental chemicals on children's health, $8.9 million to study effects of reactive oxygen species and inflammation on blood vessel function, $6.4 million to investigate better interventions against malaria, $5 million to establish a children’s environmental health center, $5.2 million to examine the connections between blood pressure regulation and Alzheimer’s disease, and $2.8 million to develop nanoparticles to treat pancreatic cancer. Read more. EHC expands urgent care and MinuteClinic options
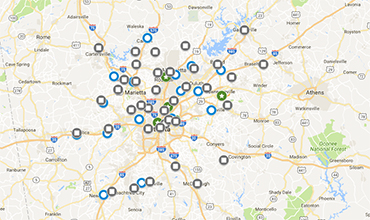
The Emory Healthcare Network (EHN) is partnering with two urgent care companies, Peachtree Immediate Care and SmartCare Urgent Care, while expanding its relationship with MinuteClinic, the retail medical clinic of CVS Health, to offer patients more options for their health care needs. These new partnerships will provide nearly 60 locations across metro Atlanta for convenient, on-demand care for patients with non-emergency needs. While staff and physicians at these locations will not be Emory Healthcare employees, the clinics will soon be linked to Emory’s electronic medical records, and patients referred to specialists within the EHN for more complex treatment will already have a health record in the system. "These clinics will allow patients to get Emory-level care in a timely manner," says EVPHA and EHC CEO Jon Lewin. "All of the urgent care clinics coming on board will have the same quality standards we hold to other members of the Emory Healthcare Network." Peachtree Immediate Care has 16 urgent care clinics in metro Atlanta and one in LaGrange. The clinics offer urgent care services for injury, flu and other illnesses, minor surgical procedures, stitches, broken bones, IV fluids, and physicals. Lab and digital X-ray capabilities are located at each site. SmartCare Urgent Care has four locations across Atlanta and offers upscale amenities such as a queuing system that allows customers to choose and hold an appointment time. MinuteClinic locations have expanded from 31 locations in 2011 to 38 today. These clinics are staffed by nurse practitioners with Emory physicians serving as medical directors. Providers specialize in family health care and can diagnose and treat common illnesses, injuries, and skin conditions. Wellness services (vaccinations, physicals, screenings) are also offered, along with monitoring for chronic conditions. Depending on their type of insurance, patients who seek care at one of these urgent care facilities can expect to pay a co-pay similar to that of a primary care visit, rather than an emergency room visit. See EHC guidelines for help in understanding what type of care is appropriate for individual needs, whether primary care, urgent care, MinuteClinic, or emergency room. Read more.
Emory emergency medicine physician Nick Colovos is medical director of strategy for the EHC urgent care and MinuteClinic partnership and worked closely with EHN and Physician Group Practice administrators, including Patrick Hammond, Matt Jernigan, Maureen Haldeman, and T.K. Everett, among others, to develop the expanded options now available to EHN patients for on-demand care. Woodruff Leadership Academy fellows announced for 2017
Following are the names of the newest fellows to participate in the Woodruff Leadership Academy, an intensive five-month leadership program, which begins its 15th year in January. Chosen through a rigorous selection process, fellows represent both faculty and staff—researchers, physicians, educators, and administrators—throughout the health sciences. Stay tuned for more information about these fellows in an upcoming issue. - Douglas Ander, Prof, Emergency Medicine; Asst Dean, Medical Education, Grady; Director, Emory Center for Experiential Learning Taking remote care a step further in the electronic ICU
When Scott Killingsworth was recovering from triple bypass heart surgery at Emory University Hospital in February, Emory's eICU team provided support that his wife, the Hon. Patricia Killingsworth, considers invaluable. "It was obvious to both of us that the team contributed greatly to the safety, continuity, and effectiveness of Scott's care, and it certainly allowed me to sleep at night knowing that the eICU team was there to work with his on-site ICU team," she says. Now, Emory's eICU has taken remote care a step further, as the team began a pilot program in mid-July from the campus of Macquarie University in Sydney, Australia. The culmination of 18 months of work and the realization of a creative vision shared by Timothy Buchman, founding director of the Emory Critical Care Center, and Cheryl Hiddleson, director of the Emory eICU Center, the idea was to turn "night into day." "We are exploring the possibilities of the future of critical care on an international platform," says Hiddleson. By using providers stationed in a complementary time zone—in this case, Sydney—to cover the Atlanta eICU night shift, it reverses two of the largest drawbacks of critical care night staffing: a shortage of senior clinicians willing to cover night shifts, and the toll that working nights takes on caretakers and their attention levels. Traditionally, says Buchman, the sickest people on the planet have rarely had a senior physician in the house at night. "There's not enough people and money available to make it happen," he says. "It shouldn't make a difference if you are sick at 2 a.m. or 7 a.m., but it does. There is a quality and safety gap." Remote electronic audiovisual monitoring of patients—the eICU—gave providers the freedom to cover a shift from off-site, but it didn't solve the night shift problem. The Australia pilot program does. Not only that, there is a waiting list of clinicians willing to cover a shift from Sydney. Participants are given time to acclimate to the time zone shift and then work for an extended period. Considerable logistical challenges had to be overcome—everything from liability issues to network connectivity to HIPAA regulations. But Hiddleson feels confident that the remote monitoring and consulting from Sydney is as secure and effective as remote monitoring by providers in the same city. "The primary responsibility still falls on the team members at the patient's bedside," she says. "We're there as a second set of eyes, with the added benefit of being able to speak directly to the bedside staff, patient, and family." The next steps will be to observe the program and its impact on patient well-being and clinician stress, as measured by cortisol levels, as well as to acquire funding. "The notion of a global eICU network is an interesting one," Buchman says. "I am having some 'what if' conversations with colleagues on what it would take to put critical care professionals shoulder to shoulder around the world, local and "visiting expatriates," so that everyone's home night-time care could be delivered from somewhere that is daylight."—Mary Loftus |
| From the Executive VP
Celebrating another year of outstanding research funding
Emory University again this year has achieved record research funding. Of the $574.6 million awarded to Emory, the Woodruff Health Sciences Center received $540 million, or 94%. What a fantastic reflection on the strength of our research teams! This is great news not only for us, but also for the people we serve and for our community. Our research programs are crucibles for discovery and innovation that significantly benefit society, and they are also boons to the local economy that bring millions of dollars in economic impact and thousands of jobs to Georgia each year. Our ability to sustain—and annually increase—such outstanding levels of funding speaks volumes about the extraordinary quality of Emory's and the Woodruff Health Sciences Center's programs and people. Thanks and congratulations to all the faculty, staff, and friends who make our continued research success possible.
Interim leaders announced
Following the recent announcement that Chris Larsen is stepping down from his positions as medical dean, Emory Clinic director, and EHC physician group president and returning to clinical practice and research, EVPHA Jon Lewin announced a series of interim appointments: David Stephens will serve as interim dean of the medical school and Ira Horowitz, as interim director of the Emory Clinic and interim physician group president. Stephens will temporarily suspend his duties as chair of the Department of Medicine, and Robert Taylor will serve as interim chair and interim chief of medicine for EHC. Monica Farley will be interim vice chair of medicine. Michael Zwick will assist Stephens in his ongoing duties as WHSC VP for research. Horowitz will temporarily suspend his duties as chair of Gyn-Ob, and Penny Castellano will serve as interim chair. New NAM members
The National Academy of Medicine (NAM) has elected Deborah Bruner (nursing) and Venkat Narayan (public health) to its 2016 class of leading health scientists. Read more. See other Emory NAM members. Check out these websites
Emory Healthcare recently debuted its newly redesigned, mobile-friendly website. Some content is still in the process of being migrated—please email the web team if you notice missing content. Also view the new "Emory at VAMC" website (www.emory.edu/vamc) for Emory faculty at the VAMC. Please email Erin Glen with any corrections. New heart surgery affiliation
The Emory Clinic's Division of Cardiothoracic (CT) Surgery has a new affiliation with St. Francis Hospital in Columbus. Emory CT surgeon Hakob Davtyan is the new medical director of St. Francis's CT surgery team. Davtyan joined the Emory faculty only recently, but he knows Emory well, having done his CT surgery training here under Robert Guyton, CT surgery division chief, who will oversee the service at St. Francis. In addition to Davtyan, two Emory-employed advanced practice providers are being added to the team at St Francis, and members of Emory's critical care and operating room staff have been deployed for some months to participate in intensive training of St. Francis staff to ensure alignment with quality and outcome metrics as the program grows. "We're bringing Emory to St. Francis," says Davtyan. Nursing partners with Atlanta Birth Center The nursing school has a new partnership with the Atlanta Birth Center, the city's only freestanding birth center, to give students experience in the birth process outside the hospital setting. Center midwives will assume an active role in the school's nurse-midwifery program, according to Carolyn Clevenger, assistant dean for MSN education. Read more. Thanking the troops
Emory University Hospital Midtown is making it easy for staff and patients to participate in a local top 40 radio station's effort to give a handwritten letter of gratitude on Thanksgiving day to every soldier deployed outside the U.S. If you'd like to participate as well, please read specifics here. The drop-off deadline for letters is Oct. 28. Please contact Min Lee if you'd like more information. Notable
Dan Brat (Winship, pathology) received a lifetime achievement award from the College of American Pathologists. Read more.
Roy Simpson (nursing school) will be inducted as a Fellow in the American College of Medical Informatics in November. Read more.
Tim Williams, EHC director of public safety, has been appointed to the Georgia Board of Private Detectives and Security Agencies by Gov. Nathan Deal. Read more. Events Nov 2: Prescribing Price: The Ethics, Science, and Business of Drug Development and Pricing. 8:15 a.m. to 3 p.m. Emory Conference Center. Register. Nov 3: The State of Child Health in Georgia. Marcus VIsiting Professor Lecture by Brenda Fitzgerald, Georgia Dept of Public Health. 4:00, HSRB auditorium. Details.
Nov 11: Veterans Day Ceremony, 11 a.m., Emory Quad. |