Hospitals achieve dramatic rise in UHC national quality rankings
Three of Emory's hospitals—Emory University Hospital (EUH), Emory University Hospital Midtown (EUHM), and Emory University Orthopaedics & Spine Hospital (EUOSH)—have made tremendous strides over the past year in national quality rankings.
| |
 |
| |
John Fox |
| |
|
| |
 |
| |
Bill Bornstein |
| |
|
| |
 |
| |
Susan Grant |
| |
|
Out of 101 academic medical centers ranked by the University HealthSystem Consortium (UHC), EUH and EUOSH (ranked jointly) jumped to 10th (up from 45th in 2010) and EUHM rose to 11th (up from 42nd in 2010).
The UHC rankings look at how academic medical centers are doing in multiple dimensions of quality and safety and are traditionally regarded as providing the best, most nonbiased national quality measurement system available. Formed in 1984, UHC is an alliance of 114 academic medical centers and 255 of their affiliated hospitals, representing approximately 90% of the nation's nonprofit academic medical centers.
Five years ago, senior leadership in Emory Healthcare added UHC data to the organization's system-wide scorecard, and since then the system has embarked on a mission to make quality improvements. This was not just to impact rankings, says John Fox, Emory Healthcare president and CEO, but more important, to redefine the care provided.
William Bornstein, chief quality and medical officer for Emory Healthcare, emphasizes that "the improvements we've achieved have been possible only through teamwork and collaboration." Susan Grant, chief nursing officer for Emory Healthcare, also emphasizes this point: "We have always known that Emory nurses, physicians, and allied health and support staff bring an unprecedented level of knowledge and expertise to patient care. Their collaboration across our system and within their teams not only has made a huge difference in our quality rankings but is changing health care for future generations." —Lance Skelly
Emory research funding totals nearly $540 million for past fiscal year
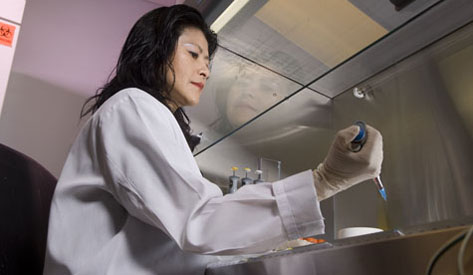 |
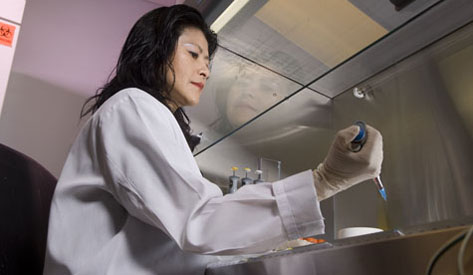
| Lily Yang is currently principal investigator on two recent grants, one exploring nanoprobes for intraoperative breast cancer margins and another to develop nanoparticles for treatment of pancreatic cancer. |
Scientists at Emory received $539.7 million from external funding agencies in fiscal year 2011, an increase from $535.1 million over the previous fiscal year. Research funding in the WHSC was $511.5 million, or more than 94% of the university total.
| |
 |
| |
David Stephens, WHSC VP for research |
David Stephens, WHSC VP for research, notes that this increase is "a remarkable achievement, in light of the current economic climate and increased competition for limited federal dollars."
About 69% of the funds, or $370.7 million, were awarded by federal agencies, led by the NIH, with $318.8 million. NIH funding represented 86% of total federal dollars awarded to Emory and more than 59% of all funding received.
Over the past five years, Emory’s research funding has increased by more than 52%.
Emory University School of Medicine received $348.4 million, or approximately 65% of the total dollars awarded. Yerkes National Primate Research Center received $70.7 million.
School of Medicine funding in the Department of Pediatrics in particular benefited from a new research partnership between Emory and Children's Healthcare of Atlanta, the Emory-Children's Pediatric Research Center. Total pediatrics extramural funding, including funding from the Children's Pediatric Research Trust, reached nearly $40 million, an increase of 57% from FY10. This included $17 million in pediatrics funding from the NIH, an increase of 10% over FY10.
The Rollins School of Public Health received $76 million, an increase of 18% over FY10, and the Nell Hodgson Woodruff School of Nursing received $10 million, an increase of 36% over last year.
Read more about individual grants received. —Holly Korschun
Getting in sync at the patient bedside
A little over a year ago, care providers on the sixth-floor medical-surgical unit at Emory University Hospital (EUH) made an important change in the morning routine of seeing patients. The entire care team, not just physicians, assembled and went together from room to room to meet as a group with each patient.
This unit, along with several others throughout Emory Healthcare, has been part of a pilot project to introduce a new tactic that was developed here at Emory and that is gaining ground nationally and internationally to enhance quality of care: structured interdisciplinary bedside rounds, or SIBR (pronounced "cyber") for short.
SIBR-ing, which takes about an hour for the entire unit, encourages questions from patients and family members, and it allows the entire multidisciplinary care team to be present for the review and planning of each patient’s daily progress.
SIBR teams include bedside nurses, nurse managers, social workers, pharmacists, palliative care specialists, and attending physicians. If other providers, such as rehab or respiratory therapists, are present at the time of rounding, they also are encouraged to participate. And because the EUH sixth floor unit is a teaching unit, the SIBR team in this case includes medical students, interns, and residents.
On each bedside round, which typically lasts about five minutes, the team follows a standard protocol and script that is constructed to ensure the following: each team member is introduced to the patient and family (and thus in the process to each other), the patient and family are given multiple opportunities to ask questions and express concerns, and checklists are run through (Does the patient have a urinary catheter? Central IV line? Pressure sores? Anticoagulant medication?) to help all team members appreciate the full scope of the patient's condition and special risk factors.
| |
 |
| |
Christina Payne |
| |
|
| |
 |
| |
Beena Sam, RN on 6G, EUH |
| |
|
| |
 |
| |
Jason Stein |
| |
|
Hospitalist Christina Payne says the SIBR model leads to better coordination of care, distributes responsibility for complex care among a larger number of people, and thus strengthens the safety net for patients. "Prior to SIBR, physicians, nurses, and other disciplines had no reliable forum to engage collaboratively with the patient," she says. "This model allows for a 360-degree approach that makes team members more aware of key quality and safety measures. This team awareness translates into actions that can reduce preventable hospital morbidity and mortality.
"SIBR also streamlines workflow," she says. "It decreases the number of pages the team receives and reduces the amount of time each discipline spends searching for care team members and family members. All of these combined allow for earlier collaboration and a smoother process for patient care.”
In addition to enhancing patient care, SIBR increases employee engagement and satisfaction, according to hospitalist Jason Stein, associate vice chair for quality for the department of medicine in the medical school, who helped inaugurate the model on the EUH unit and who is currently in Australia helping implement SIBR in several hospitals in cities throughout that country. "Foremost, the SIBR model serves the patient and the family. But it also standardizes our work, improves our reliability, fosters accountability, and helps us re-discover the professional satisfaction of caring for the patient as a team. We think the SIBR model is the future of hospital care.”
SIBR got its start at Emory two years ago, says Hal Jones, EHC care transformation director, who helped coordinate a collaborative effort led by two nursing leaders (CNO Susan Grant and associate CNO Becky Provine) and two physician leaders (clinic director Doug Morris and hospitalist Jason Stein) to launch SIBR in pilot units. "The plan eventually is to have SIBR throughout all units in all our hospitals," says Jones. "SIBR is one tactic in our overall strategy to improve quality and safety of care and patient satisfaction, and it has certainly been a contributing factor to the remarkable rankings just received by EUH and EUHM [10th and 11th, respectively] from the University HealthSystem Consortium for quality of care." —Whitney Jones and Karon Schindler
Morris appointed as clinic director
| |
 |
| |
Douglas Morris |
| |
|
Douglas Morris has been appointed as director of The Emory Clinic by the Emory University Board of Trustees. The appointment reflects Morris's exemplary leadership over the past year in the role of interim director, during which time he has managed all facets of the clinic and served as the executive physician liaison for integrating clinic physician services across Emory Healthcare hospitals and affiliates.
Morris joined the Emory faculty in 1975. Since that time, he has served Emory in many leadership roles, including director of the Emory Heart and Vascular Center and vice-chair of the Department of Medicine. He is a beloved educator, voted "Outstanding Teacher" seven years in a row by his students and earning the prestigious J. Willis Hurst Award for Excellence in Teaching in both 1995 and 2000. Atlanta Magazine has named him one of the city's "Ten Best Doctors" in cardiovascular disease every year since 1999.
"For more than three decades, Dr. Morris has demonstrated excellence as a leader in several key roles at Emory," said EVPHA Wright Caughman, "and he is highly respected as a clinician and administrator. Given his experience, his personal attributes, and his strategic knowledge of clinic operations, he is undeniably the right person for the job."
In his role as leader of Emory's physician group practice, Morris has issued a thought-provoking statement to physicians sharing his observations on the changing health care environment, the future direction of The Emory Clinic, and the actions physicians must take to ensure that Emory remains a leader in patient care and discovery. He urges doctors to lead, direct, and be prepared to adapt to change in an increasingly complex health care landscape; to embrace collaborative teamwork across disciplines; and to play a leading role in the stewardship of the health care dollar. These actions will be priorities for him in his leadership of The Emory Clinic.—Michelle Boone
A new look at 4000-year-old mummy
 |
| Emory radiologist William Torres (left) used CT imaging to allow conservators to see what was underneath the wrappings without having to disturb them. |
Where does one start putting back together a 4,000-year-old mummy whose head has fallen off and whose bones aren't where they are supposed to be? It turns out, at Emory University Hospital.
When conservators at Emory's Carlos Museum began restoration on the oldest mummy in the Western Hemisphere, now on display at the Carlos, they had many unanswered questions, according to lead conservator Renee Stein. Where were the bones located? What did they reveal about the condition of the person's health? Was the mummy male or female? What was the cause of death?
The Carlos enlisted Emory radiologist William Torres to help answer those questions about the mummy, which had lain in storage in the museum's collection since 1921. Torres used CT imaging to view the bones and their locations and prepared a 3D reconstruction that allowed the mummy to be rotated and viewed in a variety of positions. These techniques allowed the conservation team to see what was underneath the wrappings without having to disturb the fragile linens from antiquity.
Torres, who serves on the board of the Carlos and is an art collector, previously had examined a cache of mummies for an earlier Carlos exhibit that included Pharaoh Ramesses I. (Emory returned the pharaoh's mummy to Egypt in 2002 as a gesture of good will.) Unlike those mummies, which dated from the Middle Kingdom, the Old Kingdom example was in "rather bad condition," Torres says. "For one thing, the vertebral bones were in the wrong place, and the ribs were where the pelvis was supposed to be."
A combination of x-rays and CT scans showed that all the bones were well mineralized. The person had experienced no head trauma, and most likely, was male, with a large and wide skull and a brow ridge (usually lacking in women).
From the physical evidence, Emory anthropologist George Armelagos surmised that this man had enjoyed good health with access to a good diet and social advantages. The mummy's brain remains intact, with a walnut texture these 4,000 years later, and he still retains some teeth that are in amazingly good shape.
Because the mummy was buried at a holy site in Abydos, Egypt, he was likely a member of the elite class and a person of means, says Peter Lacovara, the Carlos' curator of ancient Egyptian, Nubian, and Near Eastern art. As further evidence, the base of the coffin that he rests on is made of a single piece of wood—"the cedars of Lebanon," says Lacovara—and would have been covered by a limestone sarcophagus, expenses that no ordinary Egyptian could afford.
Now through December, the mummy is the centerpiece of an exhibition at the Carlos, "Life and Death in the Pyramid Age: the Emory Old Kingdom Mummy." With a new jaw and new digits to replace missing bones from the hands and feet, he lies on his right side, as if asleep. With a reattached head supported by a headrest, he faces east to the rising sun in his afterlife. —Rhonda Mullen
For more information, see carlos.emory.edu/Old-Kingdom-Mummy. To hear a podcast by two Egyptologists discussing the Old Kingdom mummy with Carlos Curator Peter Lacovara, visit carlos.emory.edu/podcasts.
Engaging with the local community
One in a series of profiles of people in the Woodruff Health Sciences Center
When students in the Rollins School of Public Health gain access to field experiences in the community, there's a good chance that Kristin Unzicker, RSPH's director of leadership and community-engaged learning, had something to do with it. She understands the kinds of service-learning experiences these students need, in part because she used to be one herself.
Unzicker was one of the first students in RSPH's Masters International (MI) program, established in 1999 to prepare MPH students to enroll in the Peace Corps. One of her first assignments when she returned to RSPH five years ago was to expand the MI program, making it more like the Peace Corps, with a "global done local" approach to community development.
Biostats
• Current: Director, Leadership and Community Engaged Learning, Office of Admission and Student Services, RSPH
• Consultant, Curriculum Development, HERO for Children
• Peace Corps, District AIDS Coordinator, Botswana
• Manager, Education and Technology Outreach, Society for Public Health Education
• Evaluation Consultant, American Cancer Society national office
• MPH, RSPH and BS (psychology), Gustavus Adolphus College
|
|
| |
 |
| |
Kristin Unzicker |
For help, she turned to the growing number of RPCVs—returning Peace Corps volunteers—who have brought what they learned in the Peace Corps back home. In addition to mentoring and sharing their experiences with MI students, the RPCVs helped establish partnerships with local organizations serving refugees in Atlanta.
The MI students' work with local refugees through these partnerships benefits all those involved, says Unzicker. "It gives students a global experience only a few miles from their classrooms and provides much needed resources to organizations such as the Clarkston Development Foundation, Global Village School, and Refugee Resettlement and Immigration Services of Atlanta, to name a few."
The MI program has grown in recent years, and the number of RPCVs at RSPH likewise is growing, thanks to another program Unzicker helps oversee. Named for the late senator and former Peace Corps director, the Paul D. Coverdell Fellows Program offers financial assistance to RPCVs pursuing a graduate degree while working in underserved American communities. The first three fellows graduated this spring, and eight new and returning fellows are enrolled currently.
In addition to resources like the RPCVs, Unzicker works closely with Emory's Office of University-Community Partnerships, which provides funding to enhance the infrastructure at RSPH for community-engaged learning.
Unzicker makes sure that RSPH students are engaged with partner organizations in the community from virtually their first day on campus. In 2007, for example, she founded the RSPH's annual Rollins-teer Day of Service (see related item), in which every entering student is connected to a volunteer organization to help those in need. Sites have included the Atlanta Union Mission, Senior Citizens Services, Project Open Hand, and the Metro Atlanta Task Force for the Homeless. "Many students continue volunteering, sometimes interning, with the organization throughout their studies," she says.
Unzicker uses the Peace Corps's former motto, "the toughest job you'll ever love," to describe her job. She's passionate about helping a new generation of students learn while doing because, she explains, "every person with whom you connect in a community connects with other people, making even small steps exponentially great."
For her work in connecting Emory with the community, Unzicker was recognized with the 2011 Emory University Award of Distinction this past spring.
|
|
 |
|
From the Executive VP
 |
| Wright Caughman |
|
Healthy Emory, Healthy planet
The health care sector is the second largest energy consumer of all U.S. industries, but with effort and innovation, it is possible to reduce our harmful impact on the environment and do our part to advance the message “Healthy Emory, Healthy Planet.” The facilities and the sustainability initiatives of the Woodruff Health Sciences Center (WHSC) are a case in point. Sustainability has been an important part of our care experience for years, from the buildings in which we work and learn to the groundbreaking sustainability efforts being performed throughout our units.
WHSC has six LEED-certified buildings, including the Winship Cancer Institute, one of the few LEED-certified cancer centers in the country, and the Yerkes Field Station, Yerkes Neuroscience, the Whitehead Biomedical Research Building, the James B. Williams Medical Education Building, and the Emory-Children’s Center. Certification of the Claudia Nance Rollins Building is pending. LEED-certified buildings must meet high standards for energy and water conservation and indoor air quality. A significant percentage of the building materials must be recycled, renewable, or locally sourced. Research supports the health benefits of LEED-certified buildings, so ensuring that all of our facilities are healthy spaces is a priority for WHSC.
But even if you don’t happen to work or study in one of our LEED-certified buildings, there are still a wealth of sustainability initiatives going on across campus in which you can participate and of which you can be proud. For example, Emory Healthcare is changing the concept of hospital food by incorporating local and sustainable choices. We have a mercury elimination program, use reusable surgical gowns and towels, consolidate our freight deliveries to reduce traffic, reuse ice packs and Styrofoam containers from our labs, have the largest private transport fleet in Atlanta that runs on recycled cooking oil from our kitchens, and more.
These and other efforts make Emory and WHSC innovators in reducing the negative health impacts that result from climate change and energy use. Last month, Emory received a gold rating in the Sustainability Tracking, Assessment and Rating System (STARS)—a sustainability evaluation tool with broad participation from the higher education community. In fact, Emory was one of just 14 of the 170 universities registered in the program to be rated STARS gold, and the innovative buildings and cutting-edge sustainability practices here in the Woodruff Health Sciences Center were important contributors to this achievement.
Thanks for all that you do in your own unit to help promote a healthy Emory and a healthy planet.
(evphafeedback@emory.edu)
In brief
New crop of students in nursing, public health, and medicine
 |
| Nursing students at orientation |
The nursing school has 237 new students (114 BSN, 90 MSN, 28 accelerated BSN, and 5 PhD), including 22 men. The school now has 20 students overall in its doctoral program, the largest number to date.
Public health set a record for new enrollment this fall, with 530 incoming MPH and MSPH students. More than 100 of them are international students, including the first eight King Abdullah Fellows from Saudi Arabia.
The medical school welcomed 138 new students, ranging in age from 20 to 32 years. More than 60% of them are nontraditional students, with a year or more interim since attaining their bachelor's degree, and 63% hold science or engineering degrees.
New SOM master's program
 |
| Cecelia Bellcross |
|
The medical school recently launched a new Academic Health Professions Program in Genetic Counseling.
The two-year program is housed in the Department of Human Genetics and is directed by Cecelia Bellcross. The first class will be enrolled for summer 2012, and graduates will receive a master of medial science in human genetics and genetic counseling.
"While family history and genetic testing are increasingly becoming an integral part of medical care, there is a national shortage of board-certified genetic counselors who can help both the health care provider and the patient interpret genetic information related to risk," says Stephen Warren, chair of human genetics.
Haupert named CEO of Grady Health System
 |
| John Haupert |
|
John Haupert will begin his appointment as new CEO of Grady Health System in October. He most recently served as EVP and COO of Parkland Health & Hospital System in Dallas. Former Grady CEO Michael Young stepped down earlier this year to take a position in Harrisburg, Pa. A reception welcoming Haupert is scheduled for Oct. 25.
New Division of Hospital Medicine
 |
| Alan Wang |
|
The Department of Medicine has formed its 10th division, in hospital medicine. The department, which has included this specialty for more than 11 years, has the largest academic hospital medicine program in the nation. Alan Wang, who helped start the program, has been named director of the division. He will oversee the 110 faculty who cover hospital medicine in nine Emory locations.
Rollins-teers day of service
More than 500 public health students, staff, and faculty took part in public health's fifth annual Rollins-teer day of service on Aug. 18. Participants volunteered with 25 charities, including AID Atlanta, MedShare International, Senior Citizen Services, and Project Open Hand. The day gives students the opportunity to connect with the Atlanta community and experience aspects of their field that may not be apparent in traditional coursework. See related article.
Sustainability at work
Campus Services and the Environmental Health & Safety Office recently cleared out an entire floor on the Briarcliff campus previously used by the medical school. The teams were able to divert nearly 90% of the material to recycling. The recyclables filled four construction dumpsters, and only 20 to 25 bags of trash were sent to Georgia landfills. In addition, the group collected nearly four pallet-sized boxes of lab supplies that will be given to MedShare.
Notable
 |
| Susan Bauer-Wu |
A new book by Susan Bauer-Wu, Leaves Falling Gently: Living Fully with Serious and Life-Limiting Illness Through Mindfulness, Compassion, and Connectedness, offers practical guidance on using meditation for coping with serious illness. Read more.
 |
| Ann Critz |
Ann Critz, medical director of nurseries and chief of pediatrics at Emory University Hospital Midtown, was awarded the 2011 Lifetime Heroic Achievement Award from the Georgia Hospital Association for her work in neonatal intensive care over the past 30 years. Read more.
 |
| Kate Heilpern |
Kate Heilpern (chair, emergency medicine) is serving as interim chair of the family medicine department. Lawrence Lutz, founding chair of the department, stepped down Sept. 1.
 |
| Jeff Lesesne |
Jeff Lesesne (internal medicine) is the newest member of the Emory Healthcare Board. Lesesne went to medical school (class of 1996) and did residency training at Emory and has served on the faculty since that time.
 |
| Roberto Pacifici |
Roberto Pacifici (medicine) received the 2011 Louis V. Avioli Founders Award from the American Society of Bone and Mineral Research. Pacifici studied under Avioli at Washington University.
 |
| Tammie Quest |
Tammie Quest (medicine) was named director of the Emory Center for Palliative Care. She has led the center in an interim capacity since its launch in 2010. Read a recent article on palliative care at Emory.
 |
| Nanette Wenger |
Nanette Wenger (medicine) received the 2011 James B. Herrick Award for Outstanding Achievement in Clinical Cardiology from the American Heart Association Council on Clinical Cardiology.
Events
Oct. 15: Winship 5K Win the Fight Walk/Run to support cancer research and care. McDonough Field, Emory campus. Register online.
Oct. 15, 16: Juvenile Diabetes Research Foundation Walk to Cure Diabetes. Two local events, one at Centennial Olympic Park (Oct. 15) and one at State Farm Park in Johns Creek (Oct. 16). Contact Tara Davis or register online.
Oct. 20: Future Makers Lecture Series presents "Sharing Accountability through Online Care" by Jeffrey Arnold, founder of Sharecare and founder and former CEO of WebMD. More info. RSVP.
Oct. 25: Reception welcoming John Haupert, new CEO of Grady Hospital. WHSCAB, plaza level, 5-7 p.m. RSVP.
Oct. 29: American Heart Association Metro Atlanta Heart Walk. More info. |