Alzheimer's center receives $8 million grant renewal
| |
 |
| |
Allan Levey |
| |
|
| |
 |
| |
Stuart Zola |
| |
|
Emory has received renewed designation from the National Institute on Aging (NIA) as an Alzheimer's Disease Research Center (ADRC), along with a renewed five-year, $8 million P-50 grant. Emory's ADRC is the only NIA-funded center in Georgia and one of only 30 in the United States.
Faculty in medicine (neurology, pathology, psychiatry, genetics, and rehab medicine), public health, nursing, and Yerkes National Primate Research Center participate in the Emory ADRC.
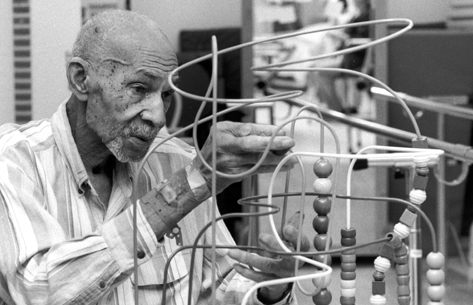
Allan Levey (chair of neurology) directs the ADRC and is principal investigator of the P-50 grant. Stuart Zola (director of Yerkes) is associate director of the ADRC and co-PI.
The Emory ADRC supports several components, including a clinical core to recruit participants and provide data on patients; a data management and statistics core to provide management of the database and biostatistical consulting to the researchers; an education and information core to educate patients, families, caregivers, general and specialty physicians, and other health care professionals; and a neuropathology core to coordinate autopsies for diagnostic assessment of brain tissue.
Emory's ADRC recruits patients from Emory and Grady Hospital for participation in the Emory ADRC registry, the autopsy program, and the various clinical research activities. Data from these cores are captured and stored for distribution to local researchers and for national collaborations. Read more.
Top
Emory's hospitals to open hospice units

Emory Healthcare is partnering with VistaCare to open hospice beds at Emory University Hospital (EUH) and EUH Midtown as an option for patient- and family-centered end-of-life care.
VistaCare, one of the largest hospice providers in the country, currently manages 24 beds at Budd Terrace skilled nursing facility at Wesley Woods Center. Fourteen of these beds will be transferred to the hospitals—eight to EUH and six to EUHM.
The eight-bed EUH hospice unit will be located on 5G. This month, 5G was closed, and patients were transferred to other EUH units, while construction was started to configure the hospice unit and reconfigure the remainder of 5G. The hospice unit is slated to open Sept. 13, and 5G to reopen with 14 beds on Nov. 1.
The six-bed EUHM hospice unit will be located on Unit 3200 in the Woodruff Building, with a targeted opening date of Sept. 1. The ante-partum unit that is currently located on Unit 3200 will move to Unit 3400 in women's health services in the Diagnostic and Treatment Center in EUHM's Medical Office Tower.
Top
Accelerated nursing degree program attracts large number of applicants
In May, the Nell Hodgson School of Nursing launched an Accelerated Bachelor of Science in Nursing (ABSN) curriculum as a second-degree program for students who have completed an undergraduate degree in a non-nursing discipline. This full-time, 15-month program includes three graduate-level courses and offers students a seamless transition into Emory's Master's of Science in Nursing program.
| |
 |
| |
Marsha Lewis |
| |
|
| |
 |
| |
Larkin Accinelli |
| |
|
"The ultimate goal of the ABSN program is to provide our students with experiences in diverse clinical settings, so they will be prepared for advanced practice nursing," says Marsha Lewis, associate dean for education in the school. "Advanced practice nurses will be more important to the health care industry in the wake of health care reform, and our ABSN students will be well prepared to step into these roles when they graduate."
The ABSN program generated more interest from prospective students than the school anticipated.
"We received more than 150 applications for the program, and we admitted 36 students," says Katie Kennedy, associate director of admission and financial aid.
The inaugural class of ABSN students range in age from 21 to 43 and come from a wide array of professional backgrounds—from supply chain management to event planning. "The new class is prepared, independent, and diverse," says Kennedy. "Many are already engaged in research."
Larkin Accinelli 11N will be among the first ABSN graduates in August 2011. She is a pre-medicine graduate of Rhodes College and was working for the World Health Organization in Argentina when she decided to apply to Emory's ABSN program.
"I was in Argentina when the swine flu rocked the country and sent everyone into an absolute panic," says Accinelli. "Being present with those people during that time and empowering the population through knowledge really cemented the fact that treating people, rather than illnesses, was important to me."
For Accinelli, Emory's ABSN program stood out among others because of its commitment to incorporating social responsibility into the curriculum.
"I love Emory's commitment to service and underserved populations. I grew up mostly overseas so I've been exposed to different cultures. I have experienced the difference health care can make in a population," Accinelli says. "I wanted a nursing program that would support my desire to practice in a not-for-profit setting and give me opportunities for rotations in these locations as well."—Jasmine Hoffman
Top
Safeguarding the human primates
One in a series of profiles of people in the Woodruff Health Sciences Center
| |
 |
| |
Maureen Thompson |
| |
|
Maureen Thompson, chief environmental health and safety officer at Yerkes National Primate Research Center, has a different perspective from that of most other managers she works with. While their focus is on the animals at Yerkes, hers is the safety and well-being of the humans who work there.
Part of Thompson's job—and that of her three-person staff—is to see that employees at Yerkes have extensive and ongoing training, personal safety equipment such as masks and gloves, immunizations, and assessments to identify health problems that could increase risk for injury or illness. Thompson and her team help employees learn ergonomics (how to lift or move heavy cages and equipment) and ways to recognize, avoid, and respond to injury or exposure to dangerous chemicals, radioactive substances, and biologic tissue or fluids.
The physical environment that Thompson oversees requires continual attention: a construction project that temporarily alters the escape plan used in fire drills, the need for proper disposal of huge amounts of biologic waste, regular laboratory inspections, and weekly testing of safety equipment, such as sinks for emergency eye wash.
Biostats:
• Environmental Health and Safety Officer, Yerkes
• Woodruff Leadership Academy alumna
• Safety Officer, Children's Healthcare of Atlanta
• Hazard Communications Program Coordinator, Children's
• Neonatal Nurse, Children's
• Neonatal Nurse, Children's Hospital of Philadelphia
• BSN, Widener Univ, Chester, Pa |
|
| |
|
The reality is that animals can be unpredictable. Even with the best training, care, and protective gear, at least a few minor bites and scratches occur every month. When such an incident occurs, Thompson directs an immediate and comprehensive response system, including around-the-clock availability of an Emory Clinic infectious disease physician.
Creating a safe environment—what Thompson calls a "culture of safety"—is what she believes is right for the center, but it's also tied to administrative requirements of Emory's Institutional Animal Care and Use Committee as well as an alphabet soup of regulatory organizations, including NIH, OSHA, EPA, CDC, and AALAC, each with its own rules about human safety. As part of the university's environmental health and safety office as well as a Yerkes manager, Thompson makes certain that safety concerns are communicated to the appropriate people and that appropriate actions are taken to uphold the university's commitment to workplace safety.
It's an ongoing challenge, one that requires constant assessment of risk and refinement of ways to decrease it. But challenge is a comfortable word for Thompson, who has climbed Mount Kilimanjaro, survived a blizzard at the base camp for Mount Everest, and is more than halfway through her personal goal to run half-marathons on all seven continents.
Top
Disaster drills probe for weak links
| |
 |
| |
Patient in decontamination unit |
| |
|
At 7:45 a.m., CNN and local TV stations began reporting large explosions near I-85 and Piedmont Road. By 8:20, first responders confirmed that hundreds of people had been exposed to Demeton-S-methyl as a result of derailment of tankers carrying the flammable pesticide. As the morning progressed, victims—many self-transported—began arriving at health care facilities all over the city, including Emory University Hospital (EUH), EUH Midtown, Wesley Woods Hospital, Emory University Orthopaedics & Spine Hospital, the Center for Rehab Medicine, and even The Emory Clinic.
Such was the scenario for last month's citywide, 23-hospital disaster drill designed to test the federal government's Chempack response and delivery system. Chempacks are medical caches of supplies available to counteract effects of chemical exposure, including exposure from possible terrorist attack.
Per Joint Commission requirements, Emory's hospitals must have a minimum of two disaster drills each year, one external drill involving other hospital systems and one internal. Since the government also requires periodic multi-hospital testing of its Chempack network, last month's drill served both government and Joint Commission mandates, according to Curtis Echols, who directs safety management and emergency preparedness for Emory Healthcare.
"The objective of the most recent drill on June 10 was to assess our hospitals' response and management when presented with strains on internal and external communication, the need for victim decontamination, patient surge, and mass fatalities," says Echols. After it was over, representatives from all 23 hospitals had a phone conference to review performance for strengths, weaknesses, and ways to improve.
"You have to train continuously to stay prepared and seek to train new staff because you lose a certain amount of this expertise due to normal staff turnover," he says.
The next series of internal drills planned for coming months will test individual hospitals at Emory, says Echols, rather than the hospitals as a group. "We'll also be testing different work shifts to make sure we're taking a global approach to expose any weak links."
Top
Emory Healthcare acquires Emory Johns Creek from HCA

Emory Healthcare and HCA announced earlier this month that Emory Healthcare will purchase HCA's ownership interest in Emory Johns Creek Hospital (EJCH) and become the sole owner of that facility, while HCA will assume full ownership of Eastside Medical Center in Gwinnett County. The partnership between the two organizations, under which these two hospitals became joint ventures, dates back to 1998.
The transition of ownership for these two hospitals is expected to be completed within the next few months. Emory Healthcare CEO John Fox says that the two organizations will work together to facilitate employee communication to provide information about the transition of payroll and other benefits.
| |
 |
| |
John Quinlivan |
| |
|
EJCH President and CEO John Quinlivan says that the hospital will continue to serve its community and support the community physicians who have been vital to its growth and development.
The 110-bed EJCH opened in 2007 and is staffed by 687 Emory and community physicians and 545 employees. Services include emergency care, digital imaging, a birth center with level III neonatal intensive care, adult intensive care, a bariatric center, advanced cardiac care, and women's services. In 2009, the hospital had 4,436 admissions and provided 45,092 outpatient services. Read more.
Top |
|
 |
|
From the Executive VP
 |
|
| Fred Sanfilippo, MD, PhD |
|
Academic health centers must lead in changing world
Bob Dylan was right: "The times, they are a-changing." Nowhere is that more true than for academic health centers (AHCs), where a variety of financial, societal, political, and demographic changes are increasingly requiring us to rethink the way we organize to achieve our lifesaving missions. Among the new realities that are converging upon AHCs are a struggling global economy, an aging Baby Boomer population that will soon flood our health care systems, a workforce shortage as health care professionals from this same generation retire, an increasing number of physicians leaving private practice, and, of course, the passage of the Patient Protection and Affordable Care Act.
The changing environment, and how AHCs should lead the response to it, was the subject of the 2010 meeting of the Blue Ridge Academic Health Group (BRAHG). Sponsored and co-led by Emory, BRAHG is composed of AHC leaders from across the nation. The group studies and makes recommendations to improve health and health care through sound research—both basic and applied—and health professional education, to help AHCs create greater value for society.
While the nation's AHCs have been through many periods of change over the past few decades, it is the unanimous consensus of BRAHG members that the current environment is truly different and unlike anything we have experienced in decades. The report based on our recent meeting will be released in coming weeks and includes recommendations for adapting to the changing environment:
• New leadership and management models. AHC leaders will need to eliminate the silo mentality in favor of enterprise thinking and accountability. Building strong teams and strategically aligning resources will be crucial to success.
• Integration/alignment. We will need to align the entire AHC—across academic and clinical units—both functionally and structurally.
• Education. We must innovate new models of education and train health professionals to work in IT-enabled settings and in coordinated inter-professional teams.
• Clinical delivery innovation. Health services research will be important in the new environment. We must innovate new models of care using a broad range of health professions to improve the quality and value of the services we provide.
• Treatment strategies. We must continue to develop new treatment strategies that take into account quality, cost, and access, and we must ensure that we have the infrastructure, especially IT, to support such strategies.
• Partnerships. We must continue to collaborate with our partners within the public and private sectors to achieve the greatest common good.
The U.S. economy, health reform, and sweeping population changes make this a unique period of both great challenge and great opportunity. It is imperative that AHCs like the Woodruff Health Sciences Center do more than just passively adapt or react to these new realities. BRAHG's recommendations this year are complex and won't be easy to achieve, but they are critical if AHCs—including the WHSC—are to meet our obligation and vision to develop proactive, effective, and innovative approaches to transforming health and healing...together.
Please share your thoughts and feedback at evphafeedback@emory.edu.
In brief
New Winship site for cancer services

Check out the newly redesigned Winship Cancer Institute website (winshipcancer.emory.edu). The site includes a comprehensive list of cancer types, with information on services, treatment, faculty, nurses, support staff, and clinical trials.
WHSC on YouTube
 Over the past 18 months, the WHSC has contributed more than 300 videos to YouTube, showcasing experts, doctors, and programs from across health sciences. Examples include Over the past 18 months, the WHSC has contributed more than 300 videos to YouTube, showcasing experts, doctors, and programs from across health sciences. Examples include
• Sustaining Haiti: Emory Medishare
• Health Impact of the Gulf Oil Disaster
• Regenerative Medicine: Steering Mother Nature
See more videos on the WHSC website video page.
U.S. News hospital rankings
Emory University Hospital was one of 152 out of 4,800 U.S. hospitals to be named in U.S. News & World Report's 2010 top 50 specialty rankings. EUH was named in 11 categories, including five in the top 20:
• Neurology/neurosurgery, 12
• Ophthalmology, 14
• Psychiatry, 15
• Kidney disorders, 16
• Heart/heart surgery, 17
• Gynecology, 22
• Geriatrics, 23
• Urology, 33
• Ear, nose, and throat, 36
• Diabetes, endocrinology, 39
• Cancer, 41
For more information, including how these rankings compare with last year's, see press release. See WHSC website for up-to-date lists of these and other rankings.
Notables
Sheila Wagner's book, Inclusive Programming for High School Students with Autism and Asperger's Syndrome, received the 2010 Outstanding Literary Award (Educational Division) from the Autism Society of America. This is the same award that her book pertaining to elementary children received previously. Wagner is assistant program director in the Emory Autism Center.
Claudia Adkison, exec. assoc. dean in the medical school, stepped down last month to begin retirement preceded by a sabbatical. She will continue to work as a consultant on special projects for the medical school. Some of her accomplishments during her past 15 years as an administrator include establishing the nine-year tenure clock, creating the faculty development policy, mentoring many faculty and chairs, establishing a "chair school" for new department heads, writing the first conflict-of-interest policies for the university and medical school, and leading the school in updating its policies on industry relationships.
Sarah Berga, chair of gyn-ob, is president nominee of the Society for Gynecologic Investigation (SGI) and will be president in 2012-2013. Robert Taylor is the current SGI president. Read more.
Emory eye researcher Jeffrey Boatwright will assume presidency of the Association for Research in Vision and Ophthalmology in 2011. Read more.
Deb Houry, director of the Emory Center for Injury Control, is president-elect of the Society for Academic Emergency Medicine (SAEM). Doug Ander and Philip Shayne are chair of the SAEM Academy of Clerkship Directors in Emergency Medicine and president of the Emergency Medicine Council of Residency Directors, respectively. Read more.
Stuart Knechtle, director of Emory's liver transplant program, has been named chief of pediatric liver transplant at Children's Healthcare of Atlanta. Read more.
Thomas Price, chief of medicine at Wesley Woods Geriatric Hospital, is one of eight practice change fellows supported by the John A. Hartford Foundation. Participants complete a project to implement a new geriatric program within their organization. Read more.
Michael Ross is president of the Society of Chest Pain Centers. Read more.
Barbara Stoll, chair of pediatrics, is currently part of the leadership of the American Pediatric Society (APS) and will be APS president in 2012-2013.
James Zaidan, chair and chief, respectively, of the anesthesiology department in the medical school and the anesthesiology service in Emory Healthcare, will step down from these positions, effective June 30, 2011, or sooner if a new chair is appointed. He will continue as a faculty member and as associate dean of graduate medical education.
Upcoming events
Sept. 28-Oct. 1: AIDS Vaccine 2010, Omni Hotel. More information. |

