Research totals by the numbers
 |
| Oncology researcher LaTonia Taliaferro-Smith is pursuing new targets for drugs that fight triple-negative breast cancer. |
Of the $481.7 million received by WHSC researchers in 2011-2012 (see EVPHA message at right), the breakdown is as follows:
The School of Medicine received $331 million, including a recent $20 million NIH grant to develop better treatments for organ transplant recipients; Rollins School of Public Health received nearly $74 million; Yerkes National Primate Research Center received $65 million; and Nell Hodgson Woodruff School of Nursing received more than $7 million.
 |
|
| David Stephens |
|
"Our research faculty deserve tremendous credit for their hard work in applying for grants and for the quality of their research that continues to attract this significant level of external funding," says David Stephens, WHSC vice president for research.
The value of biomedical research extends well beyond new cures and disease treatment and prevention, says Stephens. In Georgia, nearly 19 high-paying jobs are generated per $1 million in research funding, according to a 2011 analysis by United for Medical Research, a coalition representing leading research institutions, patient and health advocates, and private industry. And university research discoveries often are translated into commercial applications that positively impact the economy while speeding availability of medical advances to patients. Read more.
Consolidating EHC's referral base: Emory Specialty Associates
 |
| One of the larger ESA practices is in LaGrange, where the Emory Clark-Holder Clinic has 26 doctors. |
 |
|
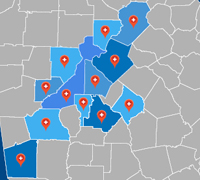
| ESA has 151 physicians in 12 counties in north Georgia. |
|
In 2006, Emory Healthcare began an outreach effort to connect with physician practices in north Georgia, particularly in metro Atlanta, consolidating them under the rubric of Emory Specialty Associates (ESA). Today ESA has grown to include 151 physicians at 38 locations and more than 735 nonphysician staff members, the latter now employees of Emory Healthcare. The largest ESA practices are in LaGrange, where the Emory Clark-Holder Clinic has 26 doctors, and in metro Atlanta, where Saint Joseph's Medical Group recently added 25 sites and 39 physicians to the ESA mix.
 |
|
| Maureen DeBlois |
|
Maureen DeBlois (pronounced de-bloy), chief administrative officer for ESA, says that such consolidation has been happening throughout Atlanta and all across the country for some time now. "With reimbursements for health services decreasing, stronger connections between physician practices and hospitals are needed to achieve efficiencies of scale and better purchasing and negotiating opportunities."
 |
|
| Richard Hansen, medical director of ESA primary care |
|
ESA physician practices "benefit from the infrastructure we provide," DeBlois explains, including back-office functions such as billing and collections, legal counsel, marketing, human resources, and finance and accounting. ESA practices also have access to EeMR, Emory's electronic medical record.
For its part, Emory Healthcare gains broader geographic reach, with ESA practices providing a feeder system for acute and specialty services. "Many ESA practices are primary care and admit patients with acute disorders like appendicitis to their local nearby hospital," she says. "We are too far away to handle needs like that. But for tertiary services and other special needs, ESA practices provide an invaluable referral network."
 |
|
| Steve Waronker, ESA division director for anesthesia |
|
Even though Emory Healthcare owns each ESA practice, the business arrangement is such that each practice rises or falls on its own bottom line. "Ten or 15 years ago when health systems acquired practices, they took away their autonomy and incentive in the process," says DeBlois. "Our compensation model is different. We pay ESA physicians on the basis of patients seen or type of work performed, which mimics the private practice model they're used to.
"We try to leverage their entrepreneurial spirit and give them the benefit of their own effort," she continues. "If they have extra cash, they can use it to reinvest in their practice—hiring extra staff or improving or expanding their facility or services." Ultimately, she adds, they determine what they need to succeed and thrive.
 |
|
| Warren Henderson, division chief for Emory Clark-Holder Clinic |
|
DeBlois says that Emory Healthcare acquires a range of practice sizes, from large to small, including one-person practices. "Our intent is to expand this network by increasing the number of physicians in some of these practices and by adding additional physician groups," she adds.
She describes Atlanta's health care market as "still very fragmented," with more independent hospitals per capita than in most large cities. "Atlanta is one of the more active cities in the country in terms of the degree of consolidation going on.
"We may not have been first to the table in the consolidation effort," she says, "but we are keeping pace. The Emory Clinic is the oldest, largest physician practice in Georgia, and the Emory name is well established."
In addition to DeBlois, other ESA leaders include Doug Morris (ESA chairman and CEO) and Don Brunn (ESA president and COO), who also serve, respectively, as CEO/director and president/COO of The Emory Clinic.
Building a resource to teach and assess clinical competency
 |
| New simulation training lab at EUHM |
This month marked the grand opening of a simulation training lab where nurses, respiratory therapists, and other providers can get hands-on practice with mock codes, sterile technique, IV placement, and other procedures in a safe, no-risk environment. Here mistakes harm no one and can benefit many, affording important opportunities for teaching and learning. The unit, located at Emory University Hospital Midtown (EUHM) but available to staff throughout Emory Healthcare, consists of a simulation room, a debriefing room where instructors and trainees can discuss what went right or wrong in each simulation scenario, and an anteroom with computers for accessing training games and resources of the Woodruff Health Sciences Library.
 |
|
| Pamela Adams |
|
According to Beth Botheroyd, manager of nursing education for Emory Healthcare, the unit exists in large part thanks to the determination and perseverance of Pamela Adams. A former staff nurse on 11 ICU at EUHM, Adams got the sim unit up and running as a project to complete her master's degree, and she recently was hired as the new unit's coordinator.
"We work with a lot of students, many of whom are amazing, but none has done anything quite like this," says Botheroyd. "Pamela had help from a lot of people, including her preceptor, Jan Whatley, but this unit was her baby. She did a really good job."
Adams may have had no budget to set up the simulation unit, but she didn't see that as a deterrent. "We put the word out about what we needed and begged, borrowed, and confiscated whatever we could, with a lot of help from facilities management," she says. "We got a bed from storage that no one had claimed and a computer monitor that someone was replacing with a new one."
The unit currently has one "static," non-interactive manikin and aspires to acquire others. "Ideally, we need more static manikins as well as low-, medium-, and high-fidelity ones," says Adams. Sometimes, she says, the unit borrows Noelle, a medium-fidelity manikin with a heartbeat, from a women's health area in the simulation unit that opened last year.
Whatever the new unit's limitations, it is nothing short of revolutionary in enhancing teaching and assessment of core competencies for nurses and other staff, says Botheroyd. "We used to rely on an annual week-long skills fair for competency training and assessment, but that didn't provide access to the kind of hands-on, one-on-one experience and feedback you can get in the sim lab."
Sharlene Toney, director of professional nursing practice and development for Emory Healthcare, agrees. "This is what hospitals have got to move forward to do," she says. "Achieving core competency is not just 'watch and do.' It's about really understanding a clinical scenario, doing the procedure correctly, and being able to critique it to understand best practice and achieve better outcomes with more efficiency."
The simulation lab is located in EUHM's Woodruff Building, Room 3209A. Regular operating hours are Monday through Friday from 8:00 to 5:00, and special arrangements can be made for evening and weekend use. Reservations can be made via the EHC intranet.
Tending a research stronghold One in a series of profiles of people in the Woodruff Health Sciences Center
 | |
| Michael Hart |
|
Emory pulmonologist Michael Hart, chief of research at the Atlanta VA Medical Center, first got hooked on VA medicine in a rotation as a medical student, and he's been involved ever since.
In fact, he turned down an NIH career development award after finishing his residency and fellowship at University of Florida to accept such an award from the VAMC in Gainesville instead.
He loves caring for veterans, "good, decent people who have made sacrifices for their country." And as a researcher, he appreciates the VA's treasure trove of patient data—one of the largest databases in the world, with information on millions of patient procedures and tests and countless embedded clues to making health care more effective and less costly.
Since Hart arrived at Emory 12 years ago, the Atlanta VAMC has experienced explosive growth. It is one the fastest growing VAMCs for new patients and has one of the 15 largest VA research programs in the country.
Hart has five active research projects himself—his specialty is vascular diseases like pulmonary hypertension that affect the lungs—and he understands the funding rules, regulations, and processes specific to the VA. Such knowledge is vital to his various research administrative roles at the VAMC, where he oversees all research done by some 150 principal investigators and their research staffs.
Like Hart, and like VAMC Chief of Staff David Bower, to whom Hart reports, the vast majority of scientists working at the VA are Emory medical faculty. A smaller number come from Emory's schools of nursing and public health, Georgia Tech, Georgia State, Morehouse School of Medicine, and other partners.
The list is likely to keep growing. Under Hart's leadership, the VA recently became a clinical site for the Atlanta Clinical and Translational Science Institute, a multi-institution alliance created to hasten translation of scientific discoveries to practical use for patients in Atlanta and beyond.
A major part of Hart's responsibilities involves administration and mentoring, helping researchers navigate often unfamiliar VA waters as they apply for funding, establish and manage laboratories, and document compliance with all federal, state, Emory, and VA regulations about safety, animal welfare, and care of patients involved in research. He has 10 staff members in the research office, including Tony Laracuente, "my right hand and three quarters of my left," an MBA-prepared, 20-plus-year VA chief administrative officer.
Currently, Hart is working to align VA resources with Emory's rapidly growing initiatives in health services research. It's a good match, he says, since health services research depends on large databases, a VA richness, rather than space, the major limiting factor on research growth in the Atlanta VAMC.
Grant supports team training for collaborative care of dying patients
The Nell Hodgson Woodruff School of Nursing has received a $1.5 million grant to train advanced practice nurses and physicians to provide collaborative care for dying patients and their families. The grant, from the Health Resources and Services Administration, a division of the U.S. Department of Health and Human Services, aims to strengthen team-based palliative care for nearly 7,000 patients over the next three years.
 |
|
| Carolyn Clevenger |
The grant will be led by geriatric nursing expert Carolyn Clevenger, a faculty member in the nursing school, in partnership with the Emory Palliative Care Center.
"Advanced practice nurses are in an ideal position to influence the patient's overall plan of care, including working with physician colleagues to provide primary palliative care," says Clevenger. "This interprofessional effort will prepare our nursing students for a team-based health care model, which is the best way to develop solutions for patients in a clinical setting."
Emergency medicine physician Tammie Quest, who directs the Emory Palliative Care Center, says that the project will pursue three objectives: to strengthen interprofessional care practice, specifically through provision of primary palliative care in selected services of Emory University Hospital (EUH); to provide expanded leadership roles for nurses at EUH; and to provide expanded opportunities for nursing students to acquire interprofessional care practice skills and knowledge. Read more.
| |
 |
|
From the Executive VP
Research success despite challenging environment
 | |
| Wright Caughman |
|
In spite of a challenging economic climate, the end of research and development under ARRA, and increased competition for increasingly limited federal research dollars, Emory University again this year exceeded half a billion dollars in research funding. Of the $518.6 million awarded to Emory, the Woodruff Health Sciences Center received $481.7 million, or 93%. While these figures represent a slight decline from last year's record-shattering totals, they still represent an outstanding level of funding success—particularly considering the challenges facing research and discovery nationwide. And the number of research proposals by Emory investigators increased significantly in FY12, which also bodes well for next year's award potential.
This marks the third year that Emory has passed the half-billion-dollar mark in research funding, which is great news not just for us, but for the state. Our research programs are crucibles for discovery and innovation, and they are boons to the local economy as well. They are helping drive recovery across the state, bringing more than $1 billion in economic impact and more than 15,000 jobs to Georgia this year. (See related story at left.)
Perhaps most impressive, we've made these strides in an environment that has been and continues to be the most challenging in recent memory. The threat of sequestration (across-the-board budget cuts) is a looming possibility, and even in the best case scenario we can look forward only to flat funding for research and development in federal budgets. The U.S. House proposes to decrease once again the salary cap for investigators, and we face increasing regulatory and compliance challenges.
Our ability to continue to sustain high levels of funding under such challenging circumstances is a direct reflection of the extraordinary quality of Emory's and the WHSC's programs and people. Our leadership, our institutional and governmental partners, and our donors recognize the promise of health-related research, and they know that Emory and its world-class team have a track record of fulfilling that promise.
Thanks and congratulations to all the faculty, staff, students, and friends who make our continued research success possible.
Please direct questions and comments to evphafeedback@emory.edu.
In brief
Ressler elected to IOM
 |
|
| Kerry Ressler |
|
Kerry Ressler (psychiatry, Yerkes) has been elected as a member of the Institute of Medicine. Ressler, who is also a Howard Hughes Medical Institute investigator, researches molecular and cellular mechanisms of fear learning and the process of extinction of fear in mouse models. He is also a practicing psychiatrist who conducts clinical research on post-traumatic stress disorder. Ressler has been principal or co-principal investigator on more than 10 NIH grants as well as multiple foundation grants. He has trained 10 PhD students and 12 postdocs.
Ressler's election brings Emory's IOM membership total to 23. Read more.
Public health and nursing each receive grants to address chronic disease
 |
|
| Venkat Narayan |
|
Researchers at the Rollins School of Public Health received a five-year, $1.1 million grant from the NIH Fogarty International Institute to create the Emory Implementation and Systems Sciences Institute. The new initiative will train 60 young investigators and leaders from India and Mexico to advance interventions and policies against chronic, non-communicable disease. Venkat Narayan, Ruth and O.C. Hubert Professor of Global Health, is the grant's lead investigator. Read more.
 |
|
| Drenna Waldrop-Valverde |
|
Meanwhile, the Nell Hodgson Woodruff School of Nursing received a five-year, $2.1 million NIH grant to establish the Center for Cognition and Affect in Chronic Illness. The new center will bring together interdisciplinary nursing research programs focused on understanding and better treating chronic illness. It will be led by nursing faculty member Drenna Waldrop-Valverde, a licensed psychologist specializing in neuropsychology whose research focuses on how chronic illnesses affect patients' brain function and ability to practice self-care. Read more.
CDC Kenya director to head Emory Global Health Institute
 |
|
| Robert Breiman |
|
The Emory Global Health Institute (GHI) has named Robert Breiman as director, effective April 2013. Breiman is currently country director for Kenya for the CDC and head of the Global Disease Detection Division for CDC-Kenya. Breiman also will hold faculty appointments in the Hubert Department of Global Health in the Rollins School of Public Health and in infectious diseases in the medical school.
Jeff Koplan, GHI founding director, will continue as VP for global health at Emory. Read more.
Email re ACA restrictions is hoax
An email spam message concerning alleged restrictions on patient care under the new Affordable Care Act (ACA) has been circulating widely in recent days. The email is a variation of an Internet hoax that has been making the rounds in several parts of the country for some months. The email describes an alleged visit to Emory by the country's "Department of Health," informing physicians that under the ACA they will be prohibited from operating on anyone over age 70 without first having approval from a board of eight doctors. Emory University has no information about where this hoax originated, but the email content is false. No government agency representatives have visited Emory or met with Emory physicians to discuss physician and patient restrictions under the ACA. Nor have there been any discussions between any Emory physicians and anyone from any government agency about withholding care from patients.
Notable
 | |
| Rebecca Gary |
|
Rebecca Gary has been named a fellow of the American Academy of Nursing. Gary, an associate professor of nursing, was one of the first nurse researchers to use exercise interventions to study diastolic heart failure in women. Read more.
 |
|
| Hanjoong Jo |
|
Hanjoong Jo, Ada Lee and Pete Correll Professor in biomedical engineering (BME), chaired the Biomedical Engineering Society's annual conference, hosted by his department in Atlanta last week. Ajit Yoganathan received the Pritzger Distinguished Lectureship Award at the meeting, and Larry McIntyre, BME department chair, was honored for his career contributions with a special symposium. Read more.
 | |
| William Kaiser |
|
William Kaiser (microbiology and immunology) received a five-year, $1.9 million NIH Early Independence Award to support his research on "programmed necrosis," a cellular process important in viral infections, inflammation, and immune disorders. Read more.
 | |
| Juan Leon |
|
Juan Leon (global health) received the 2012 Early Career in Public Health Teaching Award, presented by the Association of Schools of Public Health and Pfizer Inc. Read more.
 | |
| Nell McDonald |
|
Mary "Nell" McDonald retires next month after a 45-year career in the WHSC. She began her career at Emory in the dental school, transferred to cardiology when the dental school closed, and has been executive administrative assistant to Wayne Alexander, chair of medicine, for the past 13 years.
 | |
| Ruth Parker |
|
Ruth Parker (medicine) received the Cecilia and Leonard Doak Health Literacy Champion Award this month from Health Literacy Missouri. Read more.
 |
|
| Dennis Liotta and Ray Schinazi |
|
Ray Schinazi (pediatrics) and Dennis Liotta (chemistry) received the 2012 Intellectual Property Legends Awards from Georgia State University College of Law.
 |
|
| Susan Shapiro |
|
Susan Shapiro has been named a fellow of the American Academy of Nursing. Shapiro is assistant dean for strategic clinical initiatives in nursing and director of nursing research and evidence-based practice at Emory Healthcare. Read more.
 |
|
| Nanette Wenger |
|
Nanette Wenger (cardiology) was named a master of the American Association of Cardiovascular and Pulmonary Rehabilitation. Read more.
Events
Nov. 1: Ken Brigham and Michael M.E. Johns sign copies of their new book, Predictive health: How we can reinvent medicine to extend our best years, WHSCAB plaza level, 5 p.m. - 6:30 p.m. Read review in Wall Street Journal. Listen to the authors discuss and read excerpts from their book.
Nov. 2: Clinical Trials in Georgia: Innovations and Opportunities for Success, Academy of Medicine, Atlanta. More info.
Nov. 12: Annual Emory Veteran's Day Flag Raising ceremony, 7:45 a.m. on the quadrangle.
Nov. 15: "Health care policy and finance: What's ahead?" Michael M.E. Johns Lecture on Health Policy given by Gail Wilensky, 3:30 p.m., Claudia Nance Rollins building, 8th floor.
Dec. 6-7: 8th Annual Predictive Health Symposium. More info. |