Health Access in Ethiopia
 *photography by Nathan Golon
*photography by Nathan Golon
by Dana Goldman
The goal was to improve the everyday lives of Ethiopians by giving them access to better health services. That ambitious dream not only came true but also is spreading in new directions throughout the country and beyond.
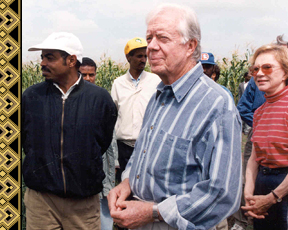
It all started in Addis Ababa, roughly 20 years ago, during a meeting between U.S. President Jimmy Carter and Ethiopian President Meles Zenawi. The two leaders and friends had just toured an agricultural demonstration project in rural Ethiopia, in which the Carter Center of Emory University was assisting. (The project later contributed to grain exports from Ethiopia for the first time in modern history.) Both men were energized by the opportunities in Ethiopia after the end of a brutal civil war. Still Zenawi knew that to stabilize his country, he needed to address a severe lack of access to health services—especially in rural areas.
|
President Carter tours a farm in Ethiopia with Prime Minister Zenawi (top left). Hailu Yeneneh (below), who served as the Carter Center’s resident technical adviser in Ethiopia, credits Emory faculty as critical in helping develop health training materials in the country. |
At the time, Ethiopia had several government-run universities that were training physicians, but most of these professionals soon left Ethiopia for better economic opportunity. Limited infrastructure, poor access to safe water, and high fertility all contributed to an already challenging situation there.
During their discussions, Carter and Zenawi agreed that any plan to train health workers and improve health conditions should be implemented by Ethiopians for Ethiopians. Their brainstorming led to the Ethiopia Public Health Training Initiative (EPHTI), launched in 1997, which set out to build a sustainable health care workforce and strengthen capacity to better tackle health needs.
“Our ultimate goal was to improve the lives of everyday Ethiopians by giving them access to better health through better trained health workers,” says Shelly Terrazas, who served as EPHTI assistant director.
Nothing like the EPHTI had previously been attempted on a national scale in a developing country. To complicate matters, the plan called for collaboration between two Ethiopian ministries—Education and Health—one which trained health workers and the other which deployed them, but these ministries had had little communication with each other.
However, the effort had several things going for it: a strong political commitment, the Carter Center’s grassroots experience in agricultural development and Guinea worm eradication, and access to Emory faculty expertise.
Over the next 13 years, the partners—including seven government-funded Ethiopian universities—focused on creating culturally appropriate and accurate health materials as well as training teachers. Colleagues from the Carter Center and Emory (led by Emory nursing professor and then-EPHTI director Joyce Murray) frequently flew to Ethiopia to train faculty counterparts there to become more effective teachers. Throughout the year, small groups of Ethiopian faculty members from around the country met to discuss health concerns and create new learning materials, a process of collaboration and open dialogue that was new for them.
Another key component of the work was providing $1 million worth of new reference materials. Many of the materials in Ethiopia’s classrooms and university libraries were decades out of date.
“When we started, the majority of faculty members were newly graduated students themselves with no experience in the classroom, and they were using notes they took as students as lesson plans because they had nothing else to work with,” says Terrazas. “We worked to strengthen their teaching skills and help them develop a comprehensive curriculum that each of the universities in the network could use.”
Fast forward to today: more than 2,500 experts have been trained through Ethiopian universities, nearly 230 health learning modules have been developed, and more than 26,000 health care professionals have been trained to serve the rural population, the majority of the population.
The EPHTI has made good on Carter’s and Zenawi’s commitments to each other. Ethiopia is now a model for a new wave of development that focuses on empowering local communities to build long-term, sustainable capacity for health services and infrastructure.
The project also has paved the way for more collaborations between Emory and Ethiopia. For instance, Emory nursing professor Lynn Sibley, who has served as an EPHTI consultant, currently is conducting a multi-year project in two rural areas of Ethiopia that helps new parents recognize signs of health problems in their newborns and connect with local health workers (see photo top left).
Perhaps most satisfying to the EPHTI team, however, is what’s happening outside of Ethiopia: the EPHTI model is spreading to other African countries. Elements of the program are being replicated in Liberia to train local health workers on mental health issues, and several African countries are working with the Carter Center on plans to create their own public health training initiatives.-EH
|
Web Connection: Through support from the Ethiopian government, all EPTHI learning materials are available for free download at: cartercenter.org/health/ephti/learning_materials/. |
*See also Educating Health Professionals in Low-Resource Countries, by Joyce Murray, Anna Frances Wenger, Elizabeth Downes, and Shelly Terrazas, on conducting teacher workshops in Ethiopia.


 *Photos: Carter Center/A. Fiorent
*Photos: Carter Center/A. Fiorent