Molecular Match Game

by Mike King, illustrations by Mark Allen Miller
In creating new drugs for chronic and neglected diseases, Emory chemists and clinicians are changing the drug discovery process—and potentially the world as we know it.
Using available space in a half-dozen buildings around campus—from undergraduate chemistry labs to Yerkes National Primate Research Center—you’d think the Emory Institute for Drug Discovery (EIDD) is having a hard time finding itself.
Not so. The three-year-old institute, one of the first and largest of its kind anywhere, is deeply grounded in a mission to change how science searches for new drugs as well as develop more effective ways of using medications already on the market. In fact, a new study in the New England Journal of Medicine finds that Emory is the fourth largest contributor in the nation to the discovery of new drugs and vaccines by public-sector research institutions.
While laboratory space for the institute may be scattered across campus, the research driving the whole enterprise is focused on one area—small molecule therapeutics. By understanding the three-dimensional structure of proteins and how they interact with each other, scientists can observe and even alter what happens within the basic building blocks of the body’s cells.

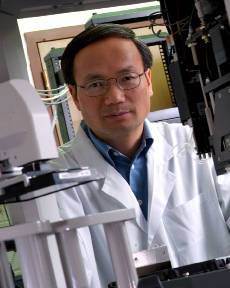
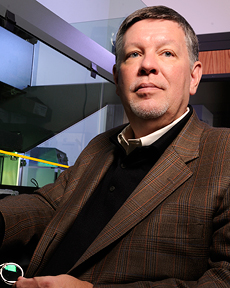
Emory researchers Dennis Liotta (left) and Ray Schinazi discovered drugs that are used routinely to treat more than 90% of patients in the United States with HIV/AIDS. |
Molecular modeling
The process amounts to a sophisticated version of an online molecular dating service using high-throughput computing, 3-D imagery, and old-fashioned trial and error. The goal is to match the molecular structure of the half-million or so compounds entered into the world’s chemical directories to the structure of proteins inside viruses, cancer cells, and other microscopic threats. Only in this case, rather than setting them up for dinner and a movie, the science matchmakers want one to change how the other does its job.
Gathering that kind of knowledge and manipulating what happens at the molecular level opens worlds of therapeutic opportunities, including potential answers for how to make anti-cancer drugs less toxic and how to interrupt the process viruses use to become resistant to anti-viral drugs. Perhaps even more significant, molecular therapeutics could hold the key in the battle against neglected diseases like malaria, tuberculosis, and dengue fever, which loom larger now that the world’s population has become more mobile and is moving from rural to urban settings.
Emory chemist Dennis Liotta, who directs the institute, is a co-inventor of drugs routinely used by more than 90% of patients in the United States being treated for HIV/AIDS. As a researcher at Emory since 1976, he’s worked with dozens of private drug companies to bring new discoveries to market, so he knows how Big Pharma works. He’s also a successful businessman who has developed several biotechnology companies of his own.
Surviving Death Valley
Liotta describes Emory’s work as critical to finding new drugs for neglected diseases that might otherwise succumb in the “valley of death” for developing drugs. That phrase describes the expensive and time-consuming phase when compounds are being tested for their safety and efficacy in laboratory animals—a time well before they reach the clinical testing stage in people.
With the average cost of developing a new drug now closing in on $1 billion, Liotta says, potential investors and even large pharmaceutical firms are often reluctant to risk money during this phase. Foundations and the government—mostly through the NIH—have until recently also declined to provide research funding during this phase of development. This problem has been particularly acute in neglected global diseases.
What’s emerging now is a new model linking global partnerships composed of small biotech labs, non-governmental organizations, foundations, government sponsors, and academic collaboratives like the EIDD. Many of those have agreements with pharmaceutical companies to jointly sponsor research.
Teaming up for global health
The institute, for example, has a collaborative arrangement with Scynexis, Inc., in Research Triangle Park, N.C., to develop an anti-viral drug for dengue fever, a mosquito-borne illness that infects 50 million people a year and causes 22,000 deaths, mostly among children. The ancient disease recently has made a comeback in places from which it had disappeared for decades. Florida state health officials reported 57 cases in 2009 and 2010, at least one of which was contracted locally.
No anti-viral treatment exists for dengue, which can have serious side effects, even though it usually is not fatal. Instead, health officials have relied on prevention efforts—mosquito nets, repellant, and removal of standing water sources that attract the insect around residences. Developing a drug to treat the illness would be a major breakthrough in global public health.
That’s a long way from happening, but this effort probably never would have been attempted under the traditional model for drug development, according to Liotta. The Emory-Scynexis relationship is rather simple, he says. “We’ll do the chemistry, and they’ll do the biology.”
Another global threat, tuberculosis, presents an even greater challenge, even though there are drugs to treat it. There are 9 million active cases annually around the world, according to the World Health Organization, and it is implicated in 2 million deaths each year. The primary issue with the effectiveness of TB drugs is patient compliance. To treat the disease effectively, TB patients must take daily medications faithfully for six to nine months. Many patients stop taking their meds after a few weeks, which has the effect of temporarily weakening the bacterium before allowing it to bounce back, stronger and more resistant to the very drugs that once worked against it. This more resistant strain of the bacterium can then be passed on to others, further complicating treatment.
With TB, the goal is to find a compound that inhibits one of the enzymes that provides energy to mycobacteria in a latent (resting) state. With such a discovery, the treatment period for TB could, in principle, be reduced to two- to three-weeks, in line with that of most other infectious diseases. That scenario, Liotta likes to say, “could change the world.”
Pooling knowledge
Emory signed a memorandum of understanding in 2010 with pharmaceutical giant GlaxoSmithKline (GSK) to become the first university to join GSK’s “intellectual property pool.” The pool targets development of new drugs for TB and other neglected diseases that plague the least developed countries. TB in particular is responsible for the death of many HIV/AIDS patients in poor countries, where the epidemic remains a major killer.
The arrangement with GSK, Liotta says, allows Emory researchers access to more than 600 patents for drugs that could be used to treat neglected diseases. Equally important, it provides EIDD scientists with direct access to their GSK counterparts. The institute is working with GSK in Tres Cantos, Spain, to screen for compounds that readily permeate the rigid clusters of TB mycobacteria, called granulomas, that make it difficult for conventional TB drugs to reach their targets.
But more than research alone, the EIDD has a compound mission—to train a new generation of scientists in drug discovery, especially among those working in developing countries. Liotta believes that the GSK agreement, and others like it, will allow the knowledge pool to expand and put drug research closer to where it is needed most.
A new world order for research
The ongoing work at Emory and other public-private collaborative drug discovery centers amounts to “an emerging new world order that holds great promise for global health,” says George Painter, chairman of the board and chief scientific officer for the biotech company Chimerix, Inc.
“The rapid movement between population centers around the world is bringing public health concerns to the forefront,” Painter says. “It’s difficult for large pharmaceutical firms to move in these global health areas because it is hard to convince near-term investors about the value of doing this type of research.”
By collaborating with centers like Emory, commercial pharmaceutical companies can reduce the risk of losing millions of dollars in research that doesn’t produce what investors want—a sure market that makes their initial investment worthwhile.
Painter, an Emory alumnus and scientific adviser for the EIDD, is enthusiastic about how quickly the public and private collaborative process for drug development is spreading. “Universities are the place where innovative research is done,” he says. “It really starts there.”
Closer to home, the EIDD is working on several major research projects aimed at new drugs and better uses of existing compounds in the fight against cancer, heart disease, and other chronic illnesses. It also has ongoing projects targeted at using compounds under development for everything from traumatic brain injury to hot flashes in menopause.
“There are so many ways where we can make a significant impact,” says Liotta, who hopes one day to have the institute’s 30 or so faculty and staff housed in one location. “Our clinicians here are so smart,” he says. “If we can just give them the tools they need, we can accomplish great things.”-EH
|
Web Connection: To see videos related to drug discovery at Emory for lung cancer, see bit.ly/lungtrial, for fragile X, bit.ly/fragilexdrug, and for cocaine addiction, bit.ly/cocainedrug. |
Match Point
Researchers across Emory’s campus are searching for drugs to treat a range of diseases from cancer and flu to infection and stroke.
InflammationOne of the compounds under development, MSX-122, has shown efficacy in animal testing for inflammation, including that seen in rheumatoid arthritis and inflammatory bowel disease, among other conditions. Drugs for arthritis are often expensive and can have serious side effects when taken on a prolonged basis. MSX-122 potentially could reduce these side effects and lower the cost of treatment. This work has progressed to the early stage of clinical testing in a small number of patients, to determine its safety. Later trials will test MSX-122’s effectiveness in larger groups of patients. CancerThe same compound, MSX-122, also may be used to reduce and possibly eliminate skin damage due to inflammation in cancer patients who are undergoing radiation therapy. Additionally, it holds the potential to be used (perhaps in pill form) by soldiers who are exposed to radiation in combat.
Emory researchers have found that UBS-109—a synthetic analog of curcumin, the major component of the spice turmeric—can be safely administered orally to retard tumor growth in mouse models for head and neck cancer. For two decades, Emory scientists have been working on safe and orally active compounds that inhibit the critical pathways associated with sphingolipid signaling, which is important for the survival, growth, and proliferation of certain types of cancer cells. The EIDD has successfully identified numerous compounds aimed at altering these sphingolipid signaling pathways in ways that might be useful for the treatment of prostate and brain cancers. With a $1.5 million grant from the National Cancer Institute, scientists at Emory’s Chemical Biology Discovery Center are studying genomic alterations in glioblastomas, the most deadly of adult brain tumors. To find a target for a new cancer drug, scientists first must find the proteins that are made by altered genes and study the interactions between those proteins within their network in a tumor. Drugs can disrupt those networks and inhibit or promote the activity of a particular target protein. To search for effective drug therapies against glioblastoma, Emory scientists will use high-throughput technologies—robotics equipment that automatically handles thousands of liquids and chemical assays in minute quantities and then computes and analyzes the resulting massive amounts of information to screen compounds against protein targets.
Fragile XEmory researchers are testing what may be the first drug therapy intended to address the complex learning and behavior problems associated with fragile X syndrome. Fragile X syndrome is caused by a genetic mutation that inhibits the production of the protein FMRP, which regulates the amount of other proteins produced in the brain. The absence of FMRP leads the glutamate receptor mGluR5 to trigger the overproduction of synaptic proteins, resulting in the learning and behavior problems characteristic of fragile X. The drug being tested for safety and efficacy in phase 2 clinical trials is an mGluR5 antagonist, which essentially puts a brake on the mGluR5 activity. The gene for fragile X was discovered in 1991 by Emory human genetics chair Stephen Warren. He led an international team that discovered the mutated gene on the X chromosome and that later developed a screening test. Infectious diseasesBesides the intensive work going on with new compounds for TB and dengue fever, Emory is deeply involved in research aimed at drug-resistant strains of HIV. Chemists working with the EIDD have identified a unique class of compounds called entry inhibitors, which may thwart the virus from penetrating uninfected cells. In collaboration with Zyrus Inc., an anti-viral drug maker located in Buford, Ga., Emory is developing a new approach that pinpoints specific host cell genes that play a role in the replication of the influenza virus. The university’s computational chemistry program is working with Zyrus to identify small molecules that modify the product of these genes to make them active anti-viral agents. Stroke and ischemic injuryEmory’s computational chemistry program and the Department of Pharmacology have discovered a series of compounds that seem to protect tissue when blood flow to the brain is interrupted, the cause of most strokes. The compounds block dysfunction in the receptors on nerve cells that cause them to die from lack of oxygen. Animal experiments have shown that they can improve therapeutic benefits and reduce the side effects typically associated with drugs to treat ischemic injury. The compounds have been licensed to NeurOP, an Atlanta biotech firm founded by Raymond Dingledine and Stephen Traynelis, two Emory researchers who have done much of the work with the compounds. Traumatic brain injuryThe work of Emory professor Donald Stein with the hormone progesterone in treating traumatic brain injury is well known. The EIDD is helping him develop a modified, soluble form of progesterone to work faster than the version now being clinically tested in patients with brain injuries. A field-ready version of progesterone could be administered by emergency medical technicians at accident scenes and by military medics on the battlefield. TransplantationThe Emory Transplant Center helped develop a new transplant immunosuppressant called belatacept, currently awaiting FDA approval. A recent trial showed that kidney transplant patients taking belatacept had graft survivals similar to those taking cyclosporine, while maintaining higher kidney function and lower blood pressure and cholesterol. In addition, belatacept can be given once every few weeks compared with twice daily dosing regimens necessary for standard immunosuppressive drugs. |
||||