News Release: Research, School of Medicine, School of Public Health
Mar. 2, 2009
Novel Pandemic Flu Vaccine Effective Against H5N1 in Mice
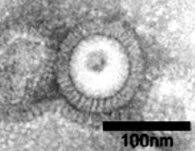 Electron microscopy of pandemic influenza H5N1 VLPs
Electron microscopy of pandemic influenza H5N1 VLPsVaccines against H5N1 influenza will be critical in countering a possible future pandemic. Yet public health experts agree that the current method of growing seasonal influenza vaccines in chicken eggs is slow and inefficient.
Scientists at the Emory Vaccine Center have developed an alternative: virus-like particles, empty shells that look like viruses but don’t replicate. Mice immunized by nose drops with the virus-like particles (VLPs) were protected for months against an otherwise lethal H5N1 infection.
The results are described in the March issue of PLoS ONE (Public Library of Science ONE).
"These results suggest that VLPs could form the basis of an effective human vaccine against H5N1 influenza,"says senior author Richard Compans, PhD, professor of microbiology and immunology at Emory University School of Medicine. Compans is director of the Emory Influenza Pathogenesis and Immunology Research Center, an Influenza Center of Excellence funded by the National Institutes of Health (NIH).
Several worldwide influenza outbreaks have occurred during the past century, with the worst being the Spanish Flu of 1918, which killed more than 50 million people.
The H5N1 variant of influenza, found among birds in Asia in the 1990s, has killed the majority of the several hundred people known to have been infected with it. Public health officials fear that H5N1, to which the human population has not developed immunity, could evolve to be transmissible between humans and cause a global pandemic with very high mortality.
Making influenza vaccines in chicken eggs poses several disadvantages. Producing vaccines takes months. Making enough for millions of people could severely stress the world’s vaccine-making capacity, especially since the poultry industry would probably be crippled in a pandemic. In addition, work with live H5N1 virus is dangerous and should only be performed in special laboratories.
As an alternative to live influenza viruses, VLPs are made by introducing three separate viral genes into baculoviruses, which only infect insect cells. Baculovirus-infected insect cells are then grown in culture, in a similar fashion to bacteria or yeast, and produce the VLPs. The VLPs appear to have a structure like influenza viruses under an electron microscope but lack the ability to replicate or to cause influenza.
Compans and first author Sang-Moo Kang, PhD, Emory assistant professor of microbiology and immunology, demonstrated the ability of VLPs to stimulate antibody production in mice. In collaboration with a team at the Centers for Disease Control and Prevention led by Ruben Donis, PhD, they showed that the mice immunized with VLPs could resist an otherwise lethal dose of H5N1 virus isolated from Vietnam.
The mice's immunity, including the levels of antibodies that protected their respiratory systems, stayed stable for over six months.
In mice, VLPs appear to deliver several times more potency per microgram than other types of vaccines, such as the chemically inactivated subunit viral vaccine currently used in the United States or a single viral protein produced in baculovirus.
"This extra potency is important because the current egg-grown vaccines require relatively high doses to be effective for most people, and in a pandemic demand might run up against production capacity. VLPs could offer more bang for the buck," Compans says.
Some next steps in the development of the vaccine are to find out if it can also protect against infection by mutant forms of the virus that arise frequently in birds, he says. Also, the vaccine will be evaluated in other animal species, in which influenza causes disease symptoms similar to those seen in humans.
Reference:
SM Kang et al. Induction of Long-term Protective Immune Responses by Influenza H5N1 Virus-Like Particles. PLoS ONE (2009).
The research was supported by the NIH and the Korean Ginseng Society.
###
The Robert W. Woodruff Health Sciences Center of Emory University is an academic health science and service center focused on missions of teaching, research, health care and public service. Its components include schools of medicine, nursing, and public health; Yerkes National Primate Research Center; the Emory Winship Cancer Institute; and Emory Healthcare, the largest, most comprehensive health system in Georgia. The Woodruff Health Sciences Center has a $2.3 billion budget, 17,000 employees, 2,300 full-time and 1,900 affiliated faculty, 4,300 students and trainees, and a $4.9 billion economic impact on metro Atlanta.
Learn more about Emory’s health sciences:
Blog: http://emoryhealthblog.com
Twitter: @emoryhealthsci
Web: http://emoryhealthsciences.org