System-wide vision for primary care |

Testing scenarios in the new EUH tower |

90-ton cyclotron for proton therapy |
 In brief |
|||||
| July 21, 2017 | |||||||||||||||||||||||||||
2017 EHC Quality Academy Awards: And the winners are. . .
Each year, teams from around Emory Healthcare submit posters highlighting their efforts to improve quality in patient care. Last year the field was expanded to include entrants from Grady, Atlanta VA Medical Center, and Children's Healthcare. The 135 entries were judged by a panel including quality experts from each institution, and 35 finalists were selected to present at Emory Healthcare's 10th annual quality conference on June 30. Nate Spell, director of the EHC Quality Academy and associate dean for education and professional development at the medical school, oversees the poster competition. He has seen the quality of the entrants evolve since its inception. "At first, we got entries that were not illustrative of quality improvement—they just showcased new devices or techniques," says Spell. "So in early years posters were judged based on application of process improvement methods rather than results." However, educational efforts across Emory Healthcare about quality improvement techniques have obviously paid off, and these days the entrants are on the mark. As a result, judging has shifted to evaluating the choice of project, appropriateness of methods, relevance of project, and the project's impact. Extra credit is given for work that is inter-professional, involves trainees, and/or works across departmental boundaries. And for the first time this year, awards were given in nine different categories, including education intervention, data analysis, quality improvement interventions, and more. View all nine winning entries.
Pratik Rachh, quality program manager in radiology in the medical school, led the team that won the Best Overall Poster for an initiative to improve chest x-ray timeliness in the ICU. Across the country, physicians in emergency departments and ICUs have adopted the practice of ordering almost every imaging study STAT, even when the designation is not actually necessary for the health of the patient. (STAT is derived from the Latin word meaning "immediately.") As a result, radiology technologists are often overwhelmed and have no way to determine which images are truly clinically urgent. Rachh and his team, which included both radiology and ICU professionals, created a new process to designate the clinically urgent image orders under very specific conditions. For orders given this designation, the technologist would be on the floor within 20 minutes to take the image, and once taken it would be read within 30 minutes. Rachh and his team rolled out the project in two EUH ICUs, and after refining it for a few months, achieved dramatic results. The average time to get an image taken dropped to 16 minutes from 70 minutes, and the average time to have the scan read dropped to 15 minutes from 520 minutes. Encouraged by the time savings, Rachh introduced the initiative to two other ICUs in March and plans to go live in two more in August. A year from now he plans to have this process in place in all EUH ICUs. "The concept is pretty straightforward," says Rachh. "It's like going to FedEx and picking either overnight delivery or two-day delivery. You are making it clear when you need that package to arrive."
In the category of Outstanding Safety Result, Ann Pekarek, director of cardiology services at EUH, led the winning team. They were able to reduce ventricular-assist device related infections to 1.5% from 7.6% through three interventions and family and patient education. Former pediatrics resident Nichole McCollum led a team of residents and nurses who won in the Outstanding Poster by Residents/Students category. They devised a method that increased the instances of nurses joining residents on their morning rounds to about 90% of the time from about 30%. Even posters that did not earn a ribbon achieved noteworthy results. A team at Grady led by Stacie Schmidt, medical director at Grady's Primary Care Center, and including David Ziemer and Yousuf Khalifa, found that only 30% of their diabetic patients had had recommended eye screenings. They purchased a retinal camera and trained medical assistants to take retinal pictures, which were sent to an ophthalmologist. If the results were abnormal, the patient was referred to the ophthalmologist. The team screened more than 2,500 patients and found that more than a third had eye pathology. "These people had not had eye care in a very long time," says Spell. "They found many patients at risk of acute vision loss. This intervention probably saved the vision of a good number of patients." "I was very impressed by the passion, sophistication, and joy reflected in the posters submitted for this year's quality conference," says Bill Bornstein, chief medical and quality officer of Emory Healthcare. "I was also struck by how far we've come in the past decade that we've been doing these conferences. We still have much to accomplish in this never-ending journey, but the work reflected in these posters bodes very well for our pursuit of the quadruple aim of better health, better experience of care, lower costs for our patients, and greater joy for our care teams."—Martha McKenzieA system-wide vision for primary care
As practitioners and payers have become smarter about ways to increase effectiveness of care and decrease costs, the importance of primary care to an academic health system like Emory has emerged as a no-brainer, key to success in population health management and to achieving the critical mass of patients needed to sustain educational and other missions.
Much is happening to invigorate primary care at Emory, thanks in part to creation three years ago of the Primary Care Consortium (PCC). Started with a WHSC innovations fund grant, the PCC is led by Ted Johnson, chair of family medicine (which includes the PA program in the medical school), and director of general medicine and geriatrics in the department of medicine. "In 2014, people involved in primary care across the system didn't know each other, whether they were doctors, nurses, or PAs, at Grady, the VA, or Emory Healthcare," says Johnson. "We needed a focal point to help integrate all primary care activities." The PCC does this by bridging all primary care efforts in the three schools and Emory Healthcare, with members meeting regularly to share best practices and playing to system-wide strengths.
Such work is aided by PCC program director Miranda Moore, who helps connect practices with health services researchers, supports efforts to achieve medical home certification, and works in general to help transition primary care at Emory from fee for service to population management. "Basically, we look to fill gaps and facilitate solutions to improve care across the board," says Moore, who has a PhD in health economics and came to Emory from the American Academy of Family Physicians.
Other key consortium members include Deena Gilland, Emory Healthcare CNO for ambulatory care services, and Carolyn Clevenger, associate dean for clinical and community partnerships in the nursing school. Their recent efforts with Johnson and others to help Emory better leverage its built-in pipeline of trainees has resulted recently in what some describe as the PCC's biggest accomplishment so far. Fixing a leaky pipeline The answer was to create a position funded jointly by the nursing and medical schools and Emory Healthcare to coordinate clinical rotations of all advanced practice provider (APP) students. With the new position, all requests for student placements were centralized through one office, with first priority for placement given to Emory students and employees. "Now, these efforts are paying off in our ability to hire our own students and retain employees," says Gilland. Similar efforts have been made to increase primary care physician recruits as well, says Johnson. "We expanded the number of faculty and residency slots in family medicine, and we're matching more Emory medical graduates as residents. We're also working to strengthen faculty development programs across general medicine." Faculty recruitment has been centralized too. Whereas in the past, different Emory primary care entities competed with one another, "now we've gone to one front door for recruitment," says Johnson. "If you want a job in the Emory Clinic or Emory Specialty Associates or general medicine at Grady, there is one set of recruiters and one application and you get one offer. We have worked aggressively to make sure we are market competitive with salary and benefits. We increased the starting salary for primary care physicians and implemented signing bonuses and programs for medical school loan repayment. We are making careers in primary care more viable and enjoyable." Looking ahead This team mindset, says Clevenger, is what will make Emory's local strategy of attaining 1 million covered lives possible. "It sounds like a lofty goal unless you remember that we're leveraging the entire health sciences center. We have all the leaders behind us and on the same page, helping set priorities and removing barriers. Once we tackle this together as a shared goal, it's relatively easy to implement," she says. Johnson sounds equally upbeat. "If you had predicted five years ago what we would have accomplished by now, people would have said, 'No way.' We have a lot more that we're looking forward to accomplishing." EUH stages scenarios to test new hospital facility
In preparation for the opening of the new Emory University Hospital tower, staff recently participated in a "Day in the Life" event, enacting scenarios in the radiology department, anesthesiology pre-admission clinic, admissions, materials management, food and nutrition, and guest services to test equipment, systems, and work flows. Watch a video of the "Day in the Life" event.
New patient routes to and from the new tower and the existing hospital were tested, with scenarios involving patients being transported across the new two-level bridge, the top level of which is dedicated specifically to patients and staff. In the new Clifton Café, food and nutrition staff reviewed procedures and processes. "The Day in the Life exercise gave hospital employees a chance to try out their new work environment and test our systems to make sure they are ready to handle patient care and flow when the first two floors open on July 31," says Bryce Gartland, EUH CEO. "Facilitators and observers worked with the staff to note issues and concerns as they arose during these scenarios." Another such event is scheduled in August.
Cancer patients, including surgical, medical oncology, and bone marrow transplant patients, will be cared for in the new tower, along with kidney, liver, and pancreas transplant patients. The hospital's medical and surgical ICUs also will be located in the new building, along with other specialties. The 450,000-square-foot, $400 million tower comprises 232 patient beds, including 40 critical care beds, adding 128 net new beds to Emory University Hospital. Floors one and two will open on July 31, along with an underground parking deck with 500 spaces. Patient floors begin opening in August, and the hospital tower will be fully operational by October. Cyclotron installed at Emory Proton Therapy Center in Midtown
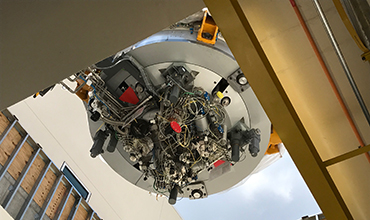
A 90-ton cyclotron was transported by truck from the port of Savannah last week and installed at the Emory Proton Therapy Center in Midtown. Watch video.
According to Mark McDonald, the center's medical director, the cyclotron accelerates proton particles to about two-thirds the speed of light to penetrate the deepest tumors in the body. The equipment is housed in a 108,000-square-foot, three-story facility that is slated to open late next year. Winship physicians, nurses, physicists, and other medical professionals will provide patient services in the facility. The approximately $200 million building and land it occupies are owned by the nonprofit Georgia Proton Treatment Center. The facility contains five treatment rooms, and when it is fully operational will serve more than 1,700 patients a year. Proton therapy is more precise than conventional forms of radiation treatment. The proton beam delivers an exact, high dose of radiation to a tumor site while sparing surrounding healthy tissue and organs from damage. Proton therapy is used to treat tumors in the brain, eye, head and neck, lung, spine, breast, and prostate. "What this means for the patient is a better chance for a cure and far fewer side effects from the therapy," says McDonald. Currently, there are about 25 proton treatment centers in this country and a total of 60 centers worldwide, with several other centers under development. Read more details about the center. |
| From the Executive VP
Our unattainable goal
Congratulations to all participants in last month's annual Emory Healthcare Quality Academy and especially to those whose projects were recognized in the poster competition. These projects addressed specific applications of broad goals for which we will always be striving—minimizing wait times, improving communication, reducing infection, prioritizing service requests, and decreasing readmissions, to name a few. Emory Healthcare has been conducting this academy for 10 years now, and over this time, categories have expanded, entries have evolved, and participants have become increasingly sophisticated at finding ways to make care better, safer, less costly, and easier to provide. But even as we get better at learning how to improve, we gain new insight into why this journey never ceases. I urge you to read about this conference in this issue and see for yourself how faculty, staff, and trainees throughout the WHSC continue to devise practical and imaginative ways to provide high-quality health care throughout our system. Please direct questions and comments to evphafeedback@emory.edu.
Top docs list
Emory physicians are well represented in the 2017 Top Doctors issue of Atlanta magazine, with 358 Emory physicians out of 720 earning recognition in the publication. Read more. New fundraising leaders for WHSC
Emory's Office of Development and Alumni Relations has appointed Mary Ann Sprinkle as VP for development and Alex Brown as Associate VP for development, both for the WHSC. Read more. Emory annual report
View the past year's accomplishments at Emory in the President's 2016 Annual Report. Huntington's reversed in mouse model
Emory researchers used CRISPR/Cas9 to disrupt a problematic gene in brain cells to reverse Huntington's disease motor symptoms in a mouse model, as reported in the Journal of Clinical Investigation. Read more. Watch video. Transplant center earns medical home recognition Emory Transplant Center is the first transplant center in the nation to earn Patient-Centered Specialty Practice (PCSP) Level 3 Recognition from the National Committee for Quality Assurance. Read more. KIds' perception influenced by genetics
Researchers at Emory, Marcus Autism Center, Children's Healthcare of Atlanta, and Washington University School of Medicine in St. Louis have found striking evidence for the role of genetics in shaping how children pay attention to the world—what they look at and what they don't. The findings have important implications for diagnosing and understanding autism. Read more. New CDC director has Emory health ties
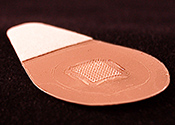
Brenda Fitzgerald, former Georgia commissioner of public health and recently appointed as CDC director, received her medical degree and postgraduate training at Emory and is an adjunct professor in Rollins School of Public Health. Read more. Microneedle vaccine patches successful
In a phase 1 trial conducted by Emory and Georgia Tech, Band-Aid-like flu vaccine patches with dissolvable microneedles were found to be safe and well tolerated by study participants. They were also found to be effective in generating immunity. The patch vaccine could increase vaccinations and save money because it is easily self-administered, could be transported and stored without refrigeration, and is easily disposed of after use without sharps waste. Read more. New Ortho & Spine clinic opens in Smyrna On July 17, Emory Healthcare opened a new outpatient clinic for orthopaedics, sports medicine, and spine treatment in Smyrna on South Cobb Drive. Read more. Stroke-protection device in TAVR
The Emory Heart & Vascular Center is among the first in the nation to offer a newly FDA-cleared device to help protect patients from stroke during transcatheter aortic valve replacement (TAVR). During TAVR and other endovascular procedures, calcium deposits or surrounding tissue can dislodge and travel to the brain. The new device is designed to filter, capture, and remove this debris before it reaches the brain. It has been shown to reduce strokes by 63% during the procedure and in the first 72 hours after the procedure, when most strokes occur. Read more. Notable
Rafi Ahmed (Emory Vaccine Center director) is one of two immunologists to receive the 2017 Robert Koch Award later this year, with prize money of 120,000 euros. The award is for pioneering research on regulation of the immune system and ground-breaking contributions to development of new vaccines and immunotherapies. Read more.
Sivan Ben-Moshe (geriatrics) and Marissa Shams (pulmonology) were named to the Atlanta Jewish Times' "40 under 40" list.
Elizabeth Corwin, associate dean for research in the nursing school, has been appointed as an Edith F. Honeycutt Chair in Nursing. Read more.
Elizabeth Downes has been named program director for the Master of Science in Nursing program in the nursing school. Read more.
Dorian Lamis (psychiatry) was named as one of "40 under 40" by the University of Georgia Alumni Association.
Tom Pearson, Emory Transplant Center director, is a new member of the board of LifeLink Legacy Fund. Read more.
Limin Peng (Biostatistics, RSPH) received the American Public Health Association 2017 Mortimer Spiegelman Award. Read more.
Peter Wilson (cardiology) received the Society of Cardiovascular Computed Tomography's 2017 Arthur S. Agatston Cardiovascular Disease Prevention Award. Read more. Events
Aug. 10: Applying Collaborative Big Data Science for Predictive Health. Part of the Think Big Symposium Series. 8 a.m. - 5 p.m. RSPH, CNR Bldg. More info. Aug. 11: Deadline to submit poster abstract for 2017 HIV & Aging: From Mitochondria to the Metropolis conference. More info.
Oct. 14: 7th annual Winship Win the Fight 5K. Atlanta Hawks star Dominique Wilkins will serve as grand marshal. More info. |