|  | |
 |
| Among the nation's most elite |  |
The Blue Ridge Institute for Medical Research has confirmed its 2018 rankings of schools and departments by NIH funding, and Emory once again scores among the nation's most elite academic health centers (AHCs). The Emory School of Medicine ranks 18th in the nation (up from 19 last year); the Nell Hodgson Woodruff School of Nursing is No. 3 in the country (up from No. 4 last year); and the Rollins School of Public Health ranks sixth nationwide. At the department level, the Woodruff Health Sciences Center had 13 in the top 20, including five in the top 10.
Individually, these school and department rankings are truly impressive achievements. Taken as a whole, they paint a picture of Emory's Woodruff Health Sciences Center as one of the top-tier research institutions in the United States. In fact, only six other AHCs in the country have top 20 ranked schools of medicine, nursing, and public health. Add Yerkes to that equation--with the largest research funding base of the seven National Primate Research Centers in the U.S.--and it's no wonder that WHSC is at the very forefront of innovation and discovery.
These rankings and all of our many research and discovery accomplishments result from the dedication of our faculty and their research teams. I'm grateful to all of you for the herculean effort you put into making this level of achievement possible.
Please direct questions and comments to evphafeedback@emory.edu.
Jonathan S. Lewin, MD, FACR
Executive Vice President for Health Affairs, Emory University
Executive Director, Woodruff Health Sciences Center
CEO, President, and Chairman of the Board, Emory Healthcare | |
| |
|  | | The Claudia Nance Rollins (2010) and Grace Crum Rollins (1994) buildings. | Rollins Foundation pledges $65 million for third RSPH building | The O. Wayne Rollins Foundation has pledged $65 million to Emory toward construction of a third Rollins School of Public Health building. To be named the R. Randall Rollins Building, the new facility will be adjacent to the existing RSPH buildings, with groundbreaking tentatively set for 2020.
The Rollins Foundation's long history of support to the RSPH includes construction of the Grace Crum Rollins and Claudia Nance Rollins buildings, opened in 1994 and 2010, respectively. RSPH has 1,164 masters and 180 PhD students and also offers non-degree courses and 12 certificate programs across various disciplines. The current buildings house six academic departments and more than 20 centers. The new building will increase the number of classrooms and faculty offices and will include state-of-the-art conferencing and distance learning space.
R. Randall Rollins is a trustee of the Rollins Foundation and chairman of the board of Rollins, Inc.; RPC, Inc.; and Marine Products Corporation. He is the son of O. Wayne and Grace Crum Rollins and grandson of Claudia Nance Rollins. Read more. | |
| |
| Teaching the educators |  | Jennifer Brandt, Taryn Taylor, Delores Lloyd |
As a rheumatologist at Grady Memorial Hospital and the Emory Clinic, Jennifer Brandt spends her days treating patients with rheumatoid arthritis, lupus, osteoarthritis, and other inflammatory diseases. She researches quality initiatives at Grady to increase patient access and improve interdisciplinary care. She also teaches rheumatology fellows and internal medicine residents in the outpatient setting.
It's the latter task for which she feels the least prepared. "Teaching is one of the most challenging but also fun parts of my job," says Brandt. "We didn't get any instruction in how to teach in medical school. As much as I enjoy it, I also wonder how I could be a more effective teacher."
So next month Brandt will join 13 other members of the Woodruff Health Educators Academy (WHEA) Teaching Fellowship to shore up those teaching skills. The group, with faculty from medicine and public health and nurses from Emory Healthcare, will meet monthly for a year to delve into topics such as lesson planning, curriculum development, teaching strategies, and assessment tools.
The new teaching fellowship grew out of WHEA's first offering, a fellowship in educational scholarship. These fellows, who are halfway through their 18-month program, have been studying education research, analyzing best methods and practices, and learning how to disseminate those research findings. When going through the applications for this inaugural fellowship, WHEA co-directors Linda Orkin Lewin and Ulemu Luhanga noticed that some of the applicants were more interested in improving their teaching skills than in doing education research, so they decided to launch a second offering.
"The Woodruff Health Sciences Center, like every academic health center, has a tripartite mission of teaching, scholarship, and service," says Luhanga, an education researcher. "However, the teaching part often does not get the recognition or support that the other two enjoy. That recognition led us to develop WHEA and the fellowships."
The teaching fellows will meet for two-hour sessions once a month to study adult learning theory, the principles of teaching, and more. Between the sessions, fellows will participate in online group discussions of practical applications for the theories they've learned. "They might talk about how to address a challenged or difficult learner, for example," says Taryn Taylor, pediatrician and director of the teaching fellowship. "Or one of the fellows might want feedback on interactive strategies to get the students involved."
For their capstone project, each fellow will create a newsletter submission summarizing his or her project. The submissions will be combined into a volume that will be available on the WHEA website as a resource for other health educators.
The teaching fellowship is unique in that it is open not only to faculty of the schools of medicine, nursing, and public health, but also to clinicians in Emory Healthcare. Delores Lloyd is such a fellow. An RN in Winship's bone marrow transplant clinic, Lloyd does not lecture in any classrooms, but she is responsible for teaching patients about their treatment plans, medications, and recovery process. "I want to learn about different educational techniques so that I might be able to develop a tool to ensure we all educate our patients in the same way and cover all the necessary topics," says Lloyd. "I'm hoping the teaching fellowship will help me improve my practice and nursing processes here."
On completing the teaching fellowship, participants will get a certificate of distinction in teaching. Graduates will also have the opportunity to teach workshops, as core faculty, to future fellowship cohorts. A call for applications for the 2020 teaching fellowship cohort will go out next fall.
The teaching fellowship and the fellowship in education scholarship are two of the key activities of WHEA. Others include an interprofessional education journal club led by Lewin; a lecture series led by Jodie Guest, professor in public health and medicine; and an online program of self-paced, guided evidence-based educator development.
"Everything we are doing at WHEA is about building and supporting an interprofessional community of educators," says Luhanga. "We want to grow the field and support the work we are passionate about."--Martha McKenzie | |
| |
| Importance of nurse mentoring |  | Jessica D'Anna and Rhonda Freeman |
Rhonda Freeman is a former high school science teacher who has channeled her skills into being an Emory nurse. Now a nurse scholar at Emory Orthopaedics & Spine Center, she sees surgical and nonsurgical patients and helps nurses there incorporate scientific evidence into their daily practice.
Working at the center is a good fit for Freeman. It allows her to pursue what she loves and maintain a schedule that allows her to spend time with her daughter after school. The latter wasn't always the case. Until recently, Freeman was nursing informatics education coordinator and an ICU nurse at Emory University Orthopaedics & Spine Hospital. While she enjoyed her work, it often required long hours that meant arriving back home well after dark.
When Freeman began contemplating a job change, she talked it over with Jessica D'Anna, the critical care nurse she is mentoring in the Emory Nurse Peer Mentoring Program (ENPMP). In this case, it was the mentor who needed some advice.
"We were talking one day when Jessica told me, 'You should think of the three things you enjoy most and let them be your priority.' I was trying to do too many things at one time and starting to feel burnout," says Freeman. "Her advice helped me transition into the role I have now."
In turn, Freeman's mentoring has proven beneficial to D'Anna as she too weighs career options and work-life balance. D'Anna joined Emory University Hospital Midtown right out of school six years ago. For the past year, she has split her time there as a CCU charge nurse and unit administrator. Recently, she began a new role in the CCU as assistant nurse manager.
"I talked to Rhonda about whether I was ready to do something really different," says D'Anna. "She helped me figure out how to twirl the baton--what to do if I said yes and what to do if I said no to an opportunity. She's helped me look at the pros and cons because she's been through these changes. That's the point of the mentoring program--to have someone to bounce your ideas off of and introduce you to different people, experiences, and opportunities."
D'Anna and Freeman are among 12 pairs of nurses piloting the 12-month ENPMP, which targets Emory Healthcare (EHC) nurses at all levels of practice and leadership. The pilot group was selected and matched by a committee of 28 EHC nurses led by Mary Zellinger, chair, and Kara Garcia, co-chair, both from Emory University Hospital. Mentors and mentees met for the first time at an inaugural meeting last spring and continue to meet as a group at quarterly meetings, where guest speakers like Sharon Pappas, EHC chief nurse executive, and Dane Peterson, EHC chief operating officer, share their own mentoring experiences. Mentors and mentees also meet on their own and touch base via phone, text, and email. A committee facilitator regularly checks in with each mentor/mentee to see how things are going.
"Everyone can benefit from a mentor, regardless of what career stage you are in," says Zellinger. "Participation in the program benefits both parties involved."
The ENPMP is modeled from evidence-based sources written by Lois Zachary, Annabelle Reitman, and Sylvia Benatti--noted career development experts--and grounded in the work of the Academy of Medical-Surgical Nurses. EUH patient family adviser Sylvia Bell also provided input, based on the peer mentoring program she developed at the CDC, where she worked for many years.
This spring, the first cohort of mentors/mentees will graduate (and continue meeting on their own), and a new cohort of mentors/mentees will be selected and matched from a pool of applications solicited by the ENPMP committee.
Long term, EHC nursing leaders would like to pair every nurse hired with a mentor. They see the ENPMP as integral to meeting EHC nursing's strategic goals of retention, healthy work environment, and engagement.
Mary Gullatte, EHC corporate director for nursing innovation and research and ENPMP executive sponsor, is a firm believer in the program. "Mentoring is about establishing a relationship with a colleague to guide and support your career goals and strengthening your connection with the organization," she says. "It's about establishing a relationship that helps you grow."--Pam Auchmutey | |
| |
|  | | First in U.S. to treat epilepsy with DBS | The Emory Brain Health Center has treated the nation’s first patient with deep brain stimulation (DBS) for drug-resistant epilepsy since commercialization of the procedure was approved last year. "DBS has been shown to significantly reduce the frequency and severity of seizures and improve quality of life out to seven years," says neurosurgeon Robert Gross, who was neurosurgical primary investigator for the SANTE trial, results of which were the basis for FDA approval of the procedure. Read more.
| | |
| | |  | | Eye care for Syrian refugees | Traveling to Syria is too dangerous, but ophthalmologists Soroosh Behshad and Natalie Weil are serving Syrian refugees at a camp in Jordan. They travel regularly to Jordan to provide surgical and clinical eye care and to educate clinicians. They work with local ophthalmologists, residents, and medical students to provide services. In January 2018, they were able to bring three of four remaining ophthalmologists out of the Syrian war zone for further education and training. Read more.
| | |
|
| |
| | 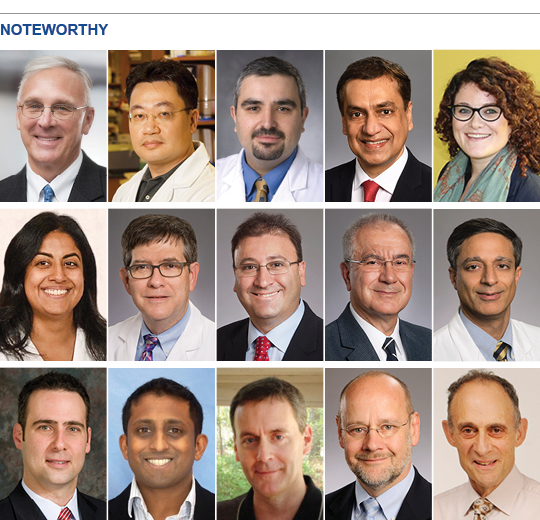 | | Michael Cassidy (director of the Emory Biomedical Catalyst) was inducted into Georgia Trend magazine's "Most Influential" Hall of Fame.
Jing Chen (hematology and medical oncology) was named the R. Randall Rollins Chair in Oncology.
Mani Daneshmand has been appointed director of the Emory Heart & Lung Transplantation and Mechanical Circulatory Support programs.
Madhav Dhodapkar (director of Winship's Center for Cancer Immunology) is the inaugural holder of the Anise McDaniel Brock Chair. He was also named a Georgia Research Alliance Eminent Scholar in Cancer Innovation.
Eva Dyer (biomedical engineering) received a research fellowship from the Alfred P. Sloan Foundation.
Reena Hemrajani (hospital medicine) is president of the Southern Region of the Society of General Internal Medicine for 2019-2020.
Dan Hunt (hospital medicine) is president-elect of the Association of Chiefs and Leaders of General Internal Medicine in 2019 and will be president next year.
Ziad Kazzi (emergency medicine) will serve on the National Council on Radiation Protection and Measurements.
Omer Kucuk (hematology and medical oncology) received the 2018 Scientific and Technological Research Council of Turkey Science Award.
Sagar Lonial (Winship chief medical officer and chair of hematology and medical oncology) recently was honored with the Anne and Bernard Gray Family Chair in Cancer.
One of neurologist Raul Nogueira's papers on thrombectomy was the most mentioned, and he was also an author on 12 of 101 top articles, as measured by Altmetrics.
Chethan Pandarinath (biomedical engineering) received a research fellowship from the Alfred P. Sloan Foundation.
Phil Rather (microbiology and immunology) was elected to the American Academy of Microbiology.
Ned Waller (hematology and medical oncology) was awarded the inaugural Rein Saral MD Professorship in Cancer Medicine.
Steven Wolf (rehabilitation medicine) is recipient of the 2019 Dean’s Distinguished Faculty Lecture and Award in the medical school. | |
| |
|  | March 5: State of the School address by Vikas Sukhatme, dean of medicine. 5:00, WHSCAB auditorium. Reception to follow.
March 21-22: Deeply Rooted:
| | |
| | | |
| |
|

