 |
|||||||||||||||||
October 2010 |
|||||||||||||||||
Class of 2011 learns the process of discoveryEighty-eight of our M4 students recently were the first to complete the Discovery phase of their training under the new medical school curriculum. "This is an intense, five-month research experience for third-year medical students that provides them an opportunity to carry out hypothesis-driven research," says Henry Blumberg (medicine and epidemiology), who, along with Maureen Powers (cell biology) is co-director of the Discovery phase. "Only a handful of medical schools in the country require this experience for medical students." Discovery starts after students complete their clinical clerkships. As part of Discovery, students participated in the weeklong course organized by Andi Shane (pediatrics) and Beau Bruce (ophthalmology). All students, regardless of the type of research project, also completed a web-based program on protection of human subjects in research. The students chose their research project after reviewing research concepts submitted by Emory faculty. According to Blumberg, "More than 300 faculty presented project ideas. The goal of Discovery is for students to help design and carry out a research study and analysis under the guidance of an Emory faculty mentor." Half of the students' mentors were faculty in surgical or medical subspecialties. The rest were scattered over a large number of departments in the SOM as well as in nursing, public health, and biomedical engineering—even creative writing. More than two-thirds of the students' projects involved human subjects research. Most students stayed at Emory, but a few completed projects at the CDC or in Washington, D.C., including one at the Department of Homeland Security. Seven students traveled internationally—to Africa (Ethiopia, Rwanda, Togo, Kenya), Peru, China, or England.
"All of the students learned that it's harder to make progress in research than they think it will be. They learned to appreciate the challenge," Blumberg says. The students will present their findings in a poster or oral presentation at Medical Student Research Day in April. A number of students will have their work published in peer-reviewed journals. "Our hope is that Discovery will help stimulate an interest and appreciation of the importance of research, whether or not the student ultimately ends up in a career that encompasses investigation," Blumberg adds. "This was the first time we presented the Discovery phase, and we believe it was very successful. Based on feedback from students and mentors we also plan to make a few revisions for enhancing it further for next year's class."
New faces of medicine prepped for successThis summer, the SOM welcomed 140 first-year medical students—76 women and 64 men. The Class of 2014 is shaping up as another high-achieving class, with an average MCAT score of 33.5. Eleven students are in the MD/PhD program, and 11 are in the MD/MPH program. Eleven students already have graduate degrees—two are dentists, two have MPH or MS/MPH degrees, two have PhDs, and five have master's degrees. The average age of the class is 23. The students have undergraduate degrees from Emory (15), University of Georgia (13), Washington University in St. Louis (10), Georgia Tech (9), University of Pennsylvania (7), Duke University (4), University of Notre Dame (4), and Amherst, Columbia, Cornell, Davidson, Georgetown, MIT, Stanford, and Yale (3 from each). In welcoming the M1 class this summer, we gave each student a copy of A Guide to Medical School Success. The booklet offers all kinds of advice, ranging from how to study to building concentration and memorization skills to managing time and priorities. The idea for the booklet came from Bill Eley, the medical school's executive associate dean for medical education, and the staff of the Benjamin Franklin Academy, a private, college-prep high school on Clifton Road. For a number of years, the academy's Wood Smethurst and Martha Burdette have been assisting medical students and residents with learning problems and reading skills. The three educators thought all first-year students could benefit from the recommendations. "This is everything I wish I had known in medical school," says Eley. "Students nowadays think they can multi-task. I tell students that doctors do not multi-task. One student recently told me that he's gone back to taking notes on paper, rather than on a laptop since it proved to be a distraction." One of the biggest nuggets in the book, Eley says, is that students should preview and review each topic for greater retention and spend at least three hours each day studying.
Fogarty scholar gains global health perspective
In August, Seema Shah 11M returned stateside from India with a greater understanding of diabetes and cardiovascular disease prevention in low-resource areas. A 2009-2010 scholar with the Fogarty International Clinical Research Scholars Program, she conducted research for nearly 11 months at the Public Health Foundation of India (PHFI) in New Dehli, one of 25 Fogarty training sites in developing countries. Shah, who will earn an MD/MPH degree in 2011, learned about the program from K.M. Venkat Narayan (medicine and RSPH epidemiology), who established a joint Emory/PHFI center in New Dehli. Narayan is principal investigator of a $3 million, five-year grant that established a Global Center of Excellence for Prevention and Control of Cardiometabolic Diseases in South Asia at the PHFI. "I was the first Emory student to start working at the site under this grant," Shah says. Her mentor, Dorairaj Prabhakaran, PHFI International Program Director, helped provide opportunities for field experience conducting clinical and translational research in diabetes management and intervention. Shah helped establish one of the site's studies, which aims to reduce cardiovascular risk among type II diabetics through the use of a care coordinator and decision-support software in clinics. She also conducted a survey of physicians who provide diabetes care in India to understand the gaps in care. "I learned that many of the challenges are the same as in the United States: increasing obesity among the population, insufficient clinic time for patients, a need for patient education, patients waiting until they have complications before seeking medical care, high-cost care, insufficient infrastructure, and not enough primary care providers." Shah continues to work on these projects and plans to implement further patient education and community-based interventions. "The Fogarty scholarship was an opportunity improve my skills in epidemiology and clinical research," she remarks, "and more importantly, learn about the on-the-ground reality of providing health care in India." New Dehli is a global site priority for the Fogarty program. Cardiovascular diseases and diabetes claim more lives in developing countries than infectious diseases. India, Pakistan, and Bangladesh are three of the top 10 countries in the world for the total number of diabetic patients and have the highest number of diabetes-related deaths. After graduation, Shah plans to pursue family and preventive medicine and continue preventive health work in India.
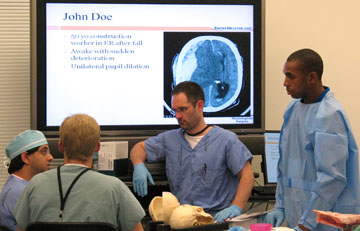
Getting into shape for neurosurgeryOur first-year neurosurgery residents got a taste of what's to come at a recent two-day national course called the Neurosurgery Boot Camp. More than 90% of all neurosurgery residency programs and postgraduate year 1 residents across the country participated in the course, which was launched by the Society of Neurological Surgeons and hosted in six cities across the country.
With equipment donated by six corporate sponsors, the residents practiced craniotomies on plastic skulls and delicate operative maneuvers on bell peppers. Attending physicians, including department chair Dan Barrow, provided lessons on basic skills needed in PGY1, such as suturing and line placement. The course focused on fundamental skills, patient safety, and communications. Day one consisted of traditional lectures, and on day two, participants performed bedside neurosurgical procedures in the simulation lab in the Williams School of Medicine Building. According to Costas Hadjipanayis, one of the Emory organizers and course directors, the 37 interns from universities across the region who participated in the Atlanta training was the largest number nationwide. "This was definitely a great start to a course we will cultivate and enhance from year to year. Our goal is for continuous evaluation and improvement," he says.
Spotlight on Family and Preventive MedicineA stronger primary care infrastructure is often cited as a needed measure to keep health care costs in check while improving care. One way to achieve that aim is through use of a team-based care model called patient-centered medical home (PCMH), a concept initially introduced by the American Academy of Pediatrics in 1967 that has received renewed attention in the wake of new health care reforms. The PCMH is designed to improve care via patient education, markers to measure outcomes, and incentives for medical practices to use it. "The Department of Family and Preventive Medicine recently opened a new clinic in Dunwoody designed to use the PCMH model and to train physicians of the future to do the same," says Lawrence Lutz, department chair. The PCMH model emphasizes a different approach to managing patients with chronic disease. Decades ago, the majority of primary care office visits were for acute problems. Today, more than three-fourths of office visits are for chronic diseases. "Yet, we still have the mentality of seeing a patient in the office, doing something, and having them leave the office with their problem 'fixed.' Three months later we see them again for the same disease and repeat the process," Lutz notes. Over the past two decades, primary care doctors have increased the number of patients seen in a day and decreased the amount of time spent per patient, Lutz says. Lifestyle issues have the greatest effect on the quality of life of patients with a chronic disease, yet they can be overlooked in a short office visit. The PCMH model specifies that patients with chronic disease be handled by teams rather than individuals. This move helps primary care physicians devote more time to managing their patients' medical problems, while topics of diet or exercise, for example, are better suited to group discussions. Each patient's health care is coordinated by the physician assistants, who also schedule quarterly team meetings to discuss patients and treatment plans, as required by PCMG. The team meets in a room with a smart board, so that patient charts can be projected, and the team can make electronic chart notations directly on the board or on a keyboard, such as reminders to make appointments for patients who need to see specialists. All the clinic's physicians use e-tablets when examining patients, and all medical records are electronic. The clinic's hallways with examining rooms are conveniently short to improve access, and the rooms are arranged around workstations. There is a preceptor room with glass so that residents can see where attending physicians are, and nurses can find PAs or doctors. The residents have computer stations near the exam rooms so they can look up medical information as they are seeing patients. The waiting rooms have patient education stations. Lutz expects the Dunwoody clinic to become a prototype for how PCMH primary care should be provided. The department's five divisions—family medicine, preventive medicine, physician assistant program, community health, and the Southeast AIDS Training and Education Center—all offer resources to the PCMH practice that non-PCMH community offices do not have.
Recent awards and honors
Maria Aaron (ophthalmology) has won the Straatsma Award for Excellence in Resident Education from the American Academy of Ophthalmology and the American University Professors of Ophthalmology. Aaron served as Emory Eye Center's Residency Program director from 1999 to 2010, during which time she trained and mentored more than 70 residents and 30 medical students. She serves on Graduate Medical Education's documents review committee, which provides oversight for all program accreditation at Emory. Claire Coles (psychiatry) was elected to the Fetal Alcohol Spectrum Disorders Study Group Advisory board, an international organization for research on these disorders. Mary Dolan (gynecology/obstetrics) was selected to serve a four-year term on the Breast and Cervical Cancer Early Detection and Control Advisory Committee of the Centers for Disease Control and Prevention. John Kim (medicine) received the American Academy of Ophthalmology Achievement Award and Scott Lambert (ophthalmology) received the American Academy of Ophthalmology Senior Achievement Award at the organization's October meeting. Jeffrey Lennox (infectious disease) has been named associate dean for clinical research in the medical school. In this new role, he leads research and work to enhance clinical trial performance throughout the school and with its many partners. He serves as section chief of infectious disease at Grady Memorial Hospital, co-director of the Clinical Research Core at the Emory Center for AIDS Research, and principal investigator of the Emory HIV/AIDS Clinical Trials Unit. Maria del Mar Sanchez (psychiatry) was appointed to the NIH Study Section for Biobehavioral Regulation, Learning and Ethology. Suresh Ramalingam (hematology and medical oncology) received the prestigious Clinical Investigator Team Leadership Award from the National Cancer Institute. This award includes a grant supplement to promote retention of outstanding clinical investigators. David Steinhauer (microbiology and immunology) was invited to serve on the editorial board for Journal of Virology. Erwin Van Meir (neurosurgery) was invited to serve as an external advisor for the five-year evaluation of the departments of neuro-oncology and neurosurgery and the brain tumor center at M.D. Anderson Cancer Center and as a reviewer for the National Medical Research Council of Singapore, the Fonds National de la Recherche, Luxemburg, and the Marie Curie fellowship grant program of the European Union. Michael Ward (ophthalmology) joined the board of directors of the Contact Lens Society of America and was appointed to the Education and Fellow Committees. He also was awarded the Beverly Myers Achievement Award for Outstanding Contributions in Ophthalmic Optics by the National Academy of Opticianry. James Zaidan (anesthesiology and associate dean of graduate medical education) was awarded the 2011 Parker J. Palmer Courage to Lead Award from the Accreditation Council for Graduate Medical Education (ACGME). The ACGME annually honors outstanding institutional officials who have created an exemplary environment for residents' ethical, professional, and personal development. | |||||||||||||||||
 |
|||||||||||||||||