If this message displays incorrectly, please view the web page

| SEPTEMBER 2016 | |||||||||||||
New Appointments
Maria Aaron (ophthalmology) was appointed associate dean for graduate medical education and is the new designated institutional official for GME.
Shawn Hochman (physiology) has been named interim chair of the Department of Physiology, beginning Sept. 1.
Nate Spell (medicine) was named associate dean for education and professional development. Notable
Anastasios Costarides (ophthalmology) received the Achievement Award from the American Academy of Ophthalmology.
Bassel El-Rayes (hematology and medical oncology) was named John Kauffman Family Professor for Pancreatic Cancer Research.
Larry Greenbaum, Marcus Professor of Pediatrics and Chief of Nephrology at Children's Healthcare of Atlanta, was named president of the American Society of Pediatric Nephrology. G. Baker Hubbard, the Thomas Aaberg Sr. Chair of Ophthalmology, received the Senior Achievement Award from the American Academy of Ophthalmology.
Veda Johnson (pediatrics) has been appointed to the Marcus Professorship in General Academics and Pediatrics. Johnson is director of Emory's PARTNERS for Equity in Child and Adolescent Health.
Yousuf Khalifa (ophthalmology) received the Achievement Award from the American Academy of Ophthalmology. He also received the Thomas M. Aaberg Teacher of the Year Award from the Emory Eye Center. Alicia Lyle (medicine) received the Early Career Investigator Award from the American Heart Association's Peripheral Vascular Disease Council. Terri McFadden (pediatrics) was named president-elect for the Georgia Chapter of the American Academy of Pediatrics.
John Pattaras (urology) was named James C. Kennedy Chair in Prostate Surgery.
Suresh Ramalingam (hematology and medical oncology), deputy director of the Winship Cancer Institute and assistant dean of research, was named Roberto C. Goizueta Chair for Cancer Research.
Peter Rossi (radiation oncology) was named James C. Kennedy Chair in Prostate Cancer. Vin Tangpricha (medicine) received the Outstanding Service Award from the American Academy of Clinical Endocrinology.
Mylin Torres (radiation oncology) was named Louisa and Rand Glenn Family Chair in Breast Cancer Research. Lary Walker (neurology) was named Marie and E.R. Snelling Professor.
Field Willingham (digestive diseases) was named president of the Georgia Gastroenterology and Endoscopic Society. William Woods (pediatrics), director emeritus of the Aflac Cancer and Blood Disorders Center, received the Aflac Cancer Center 2016 Lifetime Achievement Award. Manuel Yepes (neurology) has been named the inaugural Rollins Chair in Stroke and Imaging Research at Yerkes National Primate Research Center. Yepes is director of the Atlanta Veterans Affairs Medical Center Stroke Team. EVENTS Sixth Annual Winship Win the Fight 5K Walk/Run Oct. 1, 8:30 a.m., McDonough Field. Atlanta Braves Vice Chairman John Schuerholz will serve as grand marshal. Volunteers needed to help this Friday, Sept 30. Register here. Dean's 2016 Emory Medicine Annual Address Oct. 26, 4:30 p.m., WHSCAB Auditorium, with reception following in lobby At Grady, Oct. 27, 5:00 p.m., Faculty Office Building, room 101, with reception following. World Congress on the Prevention of Diabetes and its Complications Dec. 2-4, Georgia World Congress Center. Conference details. Emory faculty and staff receive a 10% discount with promo code: Emory10. |
|
G'day, Mate: Providing eICU care From the Other Side of the World
On July 16, at 9 a.m. Australia time and 7 p.m. Atlanta time—a key point, which will become apparent later—Emory Healthcare staff began providing remote care to Emory eICU patients from the campus of Macquarie University in Sydney. This live trial was the culmination of 18 months of work and the realization of a creative vision shared by Timothy Buchman, founding director of the Emory Critical Care Center, and Cheryl Hiddleson, director of the Emory eICU Center. The idea: Use providers to cover the Atlanta eICU night shift who are stationed in a complementary time zone where the hospital's night is their day. In other words, "turn night into day," says Buchman. “We are exploring the possibilities of the future of critical care on an international platform,” says Hiddleson. Not only are night shifts unpopular to cover, they usually fall to junior staff without the experience of senior clinicians. In addition, rotating from working days to nights takes its toll on the providers' health as well as their attention levels. "Traditionally, the sickest people on the planet have rarely had a senior physician in the house at night. There's not enough people and money available to make it happen," says Buchman. "It shouldn't make a difference if you are sick at 2 a.m. or 7 a.m., but it does. There is a quality and safety gap." Remote electronic audiovisual monitoring of patients—the eICU—gave providers the freedom to cover a shift from off-site, but it didn't solve the night shift problem. The Australia pilot program does, however. Not only that, there is a waiting list of clinicians willing to cover a shift from Sydney. Participants are given time to acclimate to the time zone shift and then work for an extended period. Considerable logistical challenges had to be overcome—everything from liability issues to network connectivity. But Hiddleson feels confident that the remote monitoring and consulting from Sydney is as secure and effective as remote monitoring by providers in the same city. "The primary responsibility still falls on the team members at the patient's bedside," she says. "We're there as a second set of eyes, with the added benefit of being able to speak directly to the bedside staff, patient, and family." The next steps will be to observe the program and its impact on clinician and patient well-being and to acquire funding. “This is extremely exciting and innovative,” says Dean Christian Larsen. “It is wonderful to see Emory critical caregivers—wide awake in the daylight—providing world-class care and support for patients during their most vulnerable periods.” For more, go to: emry.link/somcollaboration Learning About Refugee Health
A group of Emory medical students planned and hosted a Refugee Health Week recently to introduce new SOM students to refugee initiatives, including those at the Clarkston Community Health Center and refugee resettlement agencies. "Clarkston is a special place that is closer to Emory than many of us realize," says SOM student organizer Diana Jeang 19M. "The Emory Refugee Medical Alliance (ERMA), which we founded about a year ago, wanted to highlight to our student body how valuable it is to learn from the refugee community around us as well as provide an accessible means to do that." For first-year medical students, Refugee Health Week took place in their third week of school, directly after orientation and the "week on the wards." Their curriculum begins with Social Determinants of Health, so the event complemented the M1 coursework, although it was open to the entire Emory medical and public health community. The program was well attended: around 90 students registered for the events, which included a lunch talk with Dr. Alawode Oladele, medical director of countywide services for DeKalb County, on Cross Cultural Healthcare; a dinner talk and movie screening with Ngor Kur Mayol on the Lost Boys of Sudan; and Refugee Health Training Day, featuring refugees, social workers, and health care providers as guest speakers. Also, a dozen students volunteered at a service event at the International Community School. "Students got to see how multifaceted the refugee experience is and how there are countless ways to connect with the international community," Jeang says. "It was humbling to see Clarkston and Emory community members come together to make this happen." RADical Ideas
In honor of Researcher Appreciation Day (RAD) on Sept. 1, the School of Medicine recognized faculty who do groundbreaking research. The 50 researchers recognized this year were honored on emry.link/researchday. When the Emory Medicine Faculty Recognitions Committee sent out a call for nominations, it was flooded with names. "The researchers recognized represent a much broader group of Emory faculty, all of whom do inspiring and important research while mentoring, teaching, collaborating, or caring for patients," said Dean Larsen. "Emory researchers save and improve lives around the globe." The foundational and translational research conducted by those recognized included advances in ALS and Parkinson's therapies, antibiotic resistance, tumor imaging, genetics and genomics, telehealth, brain imaging, glycobiology, big data, diabetes, heart disease, stroke, lupus, Ebola, uveitis, targeted nanotechnologies, personalized medicine, pain treatment, HIV and immune dysfunction, xenotransplantation, and much more. New Hidden Gem Video: Paul Garcia
As both a practicing Emory neuroanesthesiologist and a scientist, Paul García focuses on the pharmacology involved with sedation, sleep, coma, and anesthesia. "I provide anesthesia care to patients who are undergoing neurosurgery or who have neurologic disease," he says. "My research also involves neuroscience and the brain, specifically the processing of electrical and chemical signals and the way that our anesthetic drugs interact with the brain." One of the specific areas García has worked on in recent years is hypersomnia, a disorder in which patients experience an overwhelming need to sleep and may sleep 15, 30, or even 50 hours at a stretch but are still tired on awakening. A few years ago, researchers at the Emory Sleep Center approached García requesting information about flumazenil, a drug that seems to antagonize the main inhibitory chemical of the brain, GABA. Sleep center researchers tested flumazenil on a small group of patients suffering from severe hypersomnia and saw that it helped. This led to a new line of research. "I'm very interested in using drugs like this to reverse anesthesia, because most of our anesthetic drugs work through this same receptor," says García, director of the Neuroanesthesia Laboratory at the SOM.—Wendy Darling To hear García talk about the benefit of having immigrant parents, how the brain is one of the final frontiers of science, and how a drug developed for hypersomnia might improve the reversal of anesthesia, go to emry.link/hiddengemsgarcia. Faculty Advisory Council News
At its first meeting of the year this fall, the Faculty Advisory Council (FAC) recognized the service of 2015-2016 chair Daniel Reines (biochemistry) with a glass plaque in Emory colors for his desk. "To my knowledge, it's the first time we've given a token of our appreciation to the chair, but it's a lot of work behind the scenes, and Danny did such a great job, we wanted to recognize that," says current FAC chair Mark Mullins (radiology and imaging sciences). FAC members are elected by the faculty to represent them at the SOM. Reines will continue as an ex officio member. Honoring Ken Leeper
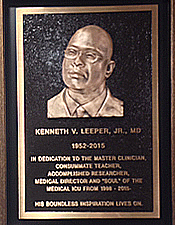
Emory pulmonologist and Professor of Medicine Kenneth Leeper believed the best outcomes in medicine come from teamwork. A year after his death at age 63, his devotion to the field is being recognized in several ways. "We will make sure that Ken Leeper's name continues to be associated with all the great teaching, patient care, and clinical research that happens at Emory University Hospital Midtown," says David Guidot (medicine), director of the Division of Pulmonary, Allergy, Critical Care, and Sleep Medicine. The Kenneth Leeper Memorial Education Fund will support clinical research and teaching at EUH Midtown as well as an annual lecture, which this April featured pulmonologist Richard Wunderink of Northwestern's Feinberg School of Medicine. Leeper's colleagues also mounted a plaque honoring his legacy in the medical ICU at Midtown. It reads: In dedication to the master clinician, consummate teacher, accomplished researcher, medical director and "soul" of the ICU from 1998-2015. His boundless inspiration lives on. "Dr. Leeper's plaque is centered on the wall above the front nurses station in 71 MICU for all to see when they enter the unit," says Debra Barker, unit director. "He was a friend to everyone and respected by all."
|