 Improving the practice of medicine Improving the practice of medicine |
 FDA approves Emory-developed drug FDA approves Emory-developed drug |
 Quicker response in system outages Quicker response in system outages |
 In brief In brief |
Emory-Georgia Tech team receives NFL grant for device to detect brain injury
 |
| Members of the iDETECT development team |
The National Football League, GE, and Under Armour have selected a team of physicians and engineers from Emory and Georgia Tech as winners of the Head Health Challenge II, a competition for new innovations intended to speed diagnosis and improve treatment for concussions.
The team received the award for development of iDETECT (integrated display enhanced testing for cognitive impairment and mild traumatic brain injury [mTBI]), a rapidly deployable system designed to improve neurologic assessment following mTBI, such as a concussion sustained in an athletic event or a military conflict.
Seven winners were selected from more than 500 submissions from 19 countries. Each team will receive $500,000 and will have the opportunity to receive an additional $1 million to advance their work.
iDETECT addresses feasibility and reliability drawbacks associated with current concussion screening tools. It is an easy-to-administer, portable system that integrates multiple concussion tests.
"A tremendous amount of research and effort has gone into the development of iDETECT, and we believe it may become an essential tool in assessing sports-related concussion," says Tamara Espinoza (emergency medicine), principal investigator of the award.
Of the 1.7 million traumatic brain injuries in the United States each year, more than 750,000 are considered "mild," and more than 173,000 are related to recreational and sports activity. In the past decade, emergency department visits for mTBI among highly vulnerable populations, such as children and developing youth, have increased by more than 60%.
The DETECT project was the brainchild of David Wright, director of Emergency Neurosciences at Emory, and Michelle LaPlaca in biomedical engineering. In 2011, the project evolved from a single neurocognitive approach for detection of concussions to an extended, multi-modal platform when the partnership broadened to include the Georgia Tech Research Institute (GTRI), which added expertise in critical systems engineering, human factors, and military medical operations.
"Mild traumatic brain injuries in youth, college, and professional sports have the potential for life-changing, long-term consequences," says Wright. "The iDETECT system allows rapid and reliable assessment at the location where the injury occurred."
In addition to Emory, Georgia Tech, and GTRI, partner institutions forming the iDETECT team include University of Rochester. The Department of Defense and the Wallace H. Coulter Foundation provided financial support.
In addition to Espinoza, Wright, and LaPlaca, team members include Shean Phelps, Brian Liu, Stephen Smith, and Courtney Crooks from GTRI; Russell Gore, sports neurologist; John Brumfield, biomedical engineer; and Jeff Bazarian, University of Rochester. Read more.
View video about iDETECT.
Improving the practice of medicine
 |
| Faculty preceptor Nate Spell with resident and patient in primary care clinic |
Judges of poster presentations for Emory Healthcare's seventh annual quality conference on October 31 received submissions from 62 health care teams reporting on methods they have applied to improve effectiveness of care in specific applications. Of these, 24 received awards, with six receiving top marks from each judge in all four grading criteria: aim statement, data, process-improvement tools, and tests of change. These six included projects to improve blood glucose control in diabetes, lipid control, RN documentation protocols in cerebral angiography, surgical site infection rates, flu vaccination rates, and timeliness of care for premature infants.
According to primary care physician Nate Spell, who led a team of residents testing a strategy to improve flu vaccination rates, the awards are based not so much on each project's results, although some had excellent results. "The scoring criteria are less about impact and more to recognize the application of process-improvement methods," says Spell, who is chief quality officer for Emory University Hospital (EUH). "In our project, we weren't teaching communication skills or even how to increase flu shots per se. We were identifying a problem, its causes, and a team strategy to address it. In an overall sense, we are helping residents understand how you do better in the practice of medicine."
Spell is one of the faculty preceptors who supervise residents in the primary care clinic in the 1525 building. "Quality improvement has been part of the residency training curriculum for some years now and is required for accreditation," says Spell. "It is an expected competency of all doctors, which is why we are working to integrate it in the undergraduate curriculum for medical students as well." He adds, "We also have an active chapter of the Institute for Healthcare Improvement Open School here at Emory, which is led by students in medicine, nursing, and public health [see related story at right]."
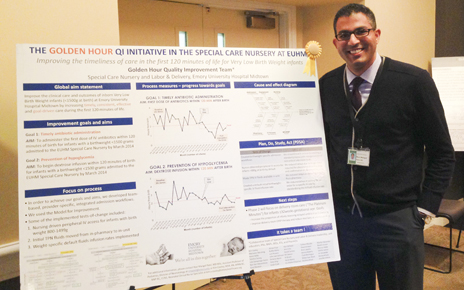 |
| A process for giving the most vulnerable newborns the best start possible |
Neonatologist Ravi Patel at EUH Midtown led a team of physicians, nurses, neonatal nurse practitioners, respiratory therapists, and pharmacists to improve the timeliness and consistency of care in the first 120 minutes of life for very low birthweight infants, those weighing less than 3 lb, 5 oz.
The team reported on phase 1 of the project, which began in April 2013 and focused on intensive care once infants are admitted to the special care nursery. The goals of this phase were to administer the first dose of antibiotics and begin IV fluids within two hours of birth, two common and vital therapies provided to preterm infants soon after they are born. "Every minute really matters for these critically ill preterm infants," says Patel. "We wanted to make sure we gave our smallest and most fragile newborns the best start possible," he adds, by improving care during what the team calls the "golden hour" and "platinum minutes" after birth.
He and his collaborators devised cause-and-effect diagrams and detailed team-based process workflows and checklists for all team members. They continuously measured their progress toward goals and showed that they were able to reduce time to initiate antibiotic therapy by 68 minutes and IV fluid infusion by 50 minutes.
Phase 2 of the project, which began in February 2014 and is still ongoing, focuses on care in the delivery room, with the goal of delaying umbilical cord clamping for 60 seconds and initiating effective CPAP therapy within 4 minutes of birth.
Bill Bornstein, chief medical and quality officer of Emory Healthcare, says, "It is very gratifying to see how skilled and sophisticated our physicians and staff have become in applying these tools to improving the care provided to our patients. These skills are at the core of how we’ve become recognized nationally for our quality of care."
FDA approves Emory-developed hemophilia drug
 |
Last month the Food and Drug Administration approved Obizur, a treatment for acquired hemophilia A that was originally developed by a research team led by Emory hematologist Pete Lollar, Hemophilia of Georgia Professor of Pediatrics. The Obizur technology was licensed by Emory in 1998 to startup company Octagen and was eventually brought to commercial availability by the pharmaceutical firm Baxter International.
 |
|
| Pete Lollar |
Hemophilia A is caused by a deficiency of clotting factor VIII and can be either inherited or acquired.
In acquired hemophilia A, the immune system is somehow provoked into making antibodies against factor VIII that inactivate it. Acquired hemophilia is a challenge for doctors to deal with because patients frequently present with severe, life threatening bleeding and also because it’s a surprise: patients do not have a previous personal or family history of bleeding episodes. Antibodies to factor VIII also can be a problem for approximately 30% of patients with inherited hemophilia.
Lollar's team developed a modified form of factor VIII, derived from the protein sequence of pigs, which is less of a red flag to the immune system.
The safety and efficacy of Obizur was evaluated in a clinical trial of 29 adults with acquired hemophilia A who received Obizur to treat a serious bleeding episode. Obizur received orphan drug designation by the FDA because the drug is intended for use in treatment of a rare disease or condition.
After licensing the technology from Emory, Octagen and a French partner, Ipsen Biopharm, pursued preclinical and clinical studies and completed a phase 2 clinical trial in 2006. Ipsen purchased the rights to the modified factor VIII in 2008 and developed a partnership with Inspiration Biopharmaceuticals in 2010. The pivotal phase 3 clinical trial took place between 2010 and 2013, and the rights to what became Obizur were bought by Baxter in 2013.—Quinn Eastman, from Lab Land
Improving response time when systems go down
 |
|
| Patrick Maloney |
A server or network outage at a facility like Yerkes National Primate Research Center is often not just a minor inconvenience but an urgent matter demanding quick resolution or workaround. Climate controls need to be maintained in animal housing, for example, frozen tissue samples need to stay frozen, animal records need to remain accessible for veterinary care, and gates should open or close as needed.
Information technology manager Patrick Maloney recently led a team that developed a new process for handling major incidents affecting critical business services at Yerkes. The result is a much quicker turnaround time to resolve major incidents, and Yerkes personnel are now serving as a resource to other units across campus that are developing and implementing similar response procedures.
To devise the new process, Maloney and his team worked with service desk manager Sharon Gregory and her team at the university-wide Libraries and Technology Services, or LITS, over a 15-month period. During this time, the team determined what qualified as a major incident, identified who needed to be notified based on the incident, trained staff, and tested the process. Yerkes implemented the new system earlier this year.
"We worked with LITS and documented steps along the way so people could reference them going forward," says Maloney. "Now if I have an issue, I can report an outage, and LITS staff can page their on-call folks and respond within an hour. The new process has dramatically improved the continuity of IT operations at Yerkes. In addition, LITS now has a better understanding of our animal care needs and the accessibility and protection of our critical research data.”
Yerkes was the first unit to implement a major incident process outside of LITS. Since then, the Emory Service Management Competency Center asked Maloney and Tanisha Hill of Goizueta Business School to meet with other Emory incident managers to expand the major incident process. According to Maloney, he and Hill have met with incident managers from Candler School of Theology, Emory Alumni Association, Rollins School of Public Health, Department of Psychology in Emory College, and administrative units in the medical school.
“With the new system in place at Yerkes, it took only 10 minutes to begin addressing the first reported concern, something that previously may not have been addressed for as long as two days,” says Maloney. “We’ve increased our efficiency and therefore customer satisfaction, and we’re available to help other Emory units do the same.”—Lisa Newbern
Responding to people's needs
 |
|
| Wright Caughman |
Emory has received intense media coverage recently for its leadership role in treating patients with Ebola virus disease (EVD). And it's true that our clinical, educational, research, and advocacy activities around EVD have been extraordinary. We're recognized as a leader in the effort to eradicate EVD, and our work is making a global impact. And yet, a recent publication reminds us that this lifesaving work represents only a fraction of the good we do—one disease among many, a handful of patients among thousands.
The 2014 Community Benefits Report highlights many of the other ways in which we've touched people's lives over the past year. In fiscal year 2014, Emory provided more than $85 million in charity care—an increase of 6% over 2013, and an increase of more than 18% since fiscal year 2012. These increases in charity care are a direct response to the needs of the people we serve—some who are uninsured, some who are underinsured, and some for whom the cost of extensive care would be catastrophic.
These and other numbers in this year's Community Benefits Report are impressive without a doubt. The stories of some of the real beneficiaries of our care are deeply moving and remind us why what we do is so crucial and so rewarding. As we enter the season of gratitude, I'm grateful to belong to an institution that is not only on the leading edge of a high-profile global fight, but that is also making an immeasurable impact right here in our community. Thanks to all of you for making a difference for the people we serve, and best wishes for a happy Thanksgiving.
Please direct questions and comments to evphafeedback@emory.edu.
|
 |
Training students in quality improvement
 |
|
| Ariadne DeSimone |
The Emory chapter of the Institute for Healthcare Improvement Open School recently developed and conducted a Healthcare Quality Improvement Training Day, held on Nov. 8. This interprofessional session was led by chapter student board members Ariadne DeSimone (public health), Tana McCoull (nursing), and Erin Bredenberg (medicine) with the support of seven other board members, including chapter president, Byron Crowe.
 |
|
| Anne Tomolo |
Anne Tomolo, chief of quality medicine at the Atlanta VA Medical Center and site director for postgraduate training in quality and safety, and her fellows and chief resident assisted the group in planning and facilitating this event, which was attended by 43 students in medicine, nursing, public health, and allied health and incorporated both didactic and experiential learning.
Patient satisfaction commendations
In his annual Emory Medicine address last month, medical dean Chris Larsen commended the following faculty in medicine and ophthalmology who scored at or above the 90th percentile on Press Ganey patient satisfaction surveys in every quarter of FY 2014, with each physician receiving more than 30 surveys per quarter:
Medicine (All are in primary care except as otherwise noted.)
Monica Agrawal, Paul Baird, Sharon Bergquist, Elizabeth Billinsgley, Brenton Black, Jerard Cranman, Donald Davis, Priya Dayamani (endocrinology), Jean Fiedler, Thomas Jarrett, Meekyung Kim, Jonathan Masor, Gerard McGorisk (cardiology), Jennifer Morgan, David Propp, Laurence Sperling (cardiology), Dipak Vashi, Sally West, Jennifer Zreloff
Ophthalmology
Maria Aaron, Fulya Anderson, Mary Carlton, Ann Van Wie
PCORI grant for studying patient consent in acute settings
 |
A research team led by cardiologist Neal Dickert received a $1.07 million award from the Patient-Centered Outcomes Research Institute to develop processes for involving patients and family members in decisions about enrollment in clinical trials in the setting of acute conditions like heart attack and stroke. Read more.
For the fourth consecutive year, Emory University Hospital (EUH) ranked in the top 10 in the University HealthSystem Consortium annual awards. (See other awardees.) EUH ranked eighth, and EUH Midtown ranked 22nd. Both hospitals were in the top 10 in 2012 and 2013, and Emory Healthcare is still the only organization ever to have two hospitals rank so highly.
Performance of all UHC member hospitals has been rising dramatically, which makes the rankings ever more challenging, but means that more patients are benefiting from enhanced quality of care. Ranking methodology also changes annually, so while a hospital may be holding firm in one category, the methodology continues to evolve and the bar continues to rise, also good for patients. Note: All data periods for the 2014 rankings were complete by June 2014 and were unaffected by Emory's extraordinary efforts in caring for patients with Ebola virus disease.
Veterans at Emory
 |
According to a page on Emory's Human Resources website, there are at least 254 veterans employed by the university and 324 employed by Emory Healthcare. More than a third are in leadership positions. One of these is Andrew West, a Marine Corps reservist and senior administrator in the Atlanta Clinical and Translational Science Institute, who recently returned to this position from a tour in Afghanistan as a mobility chief with a logistics unit. (Photo by US Army veteran Kristina Ortiz, research specialist in pathology)
Notable
 |
The Jean and Paul Amos Parkinson's Disease and Movement Disorders Program, led by neurologist Stewart Factor, has been designated a Center of Excellence by the National Parkinson Foundation (NPF). NPF has designated 40 such centers around the world and provides grant funding to them. Read more.
 |
Mary Gullatte, currently CNO at Emory University Hospital Midtown, has been appointed corporate director of nursing innovation and research for Emory Healthcare. She will assume her new responsibilities full time at the beginning of the year. June Connor, CNO/COO at Emory University Orthopaedic & Spine Hospital, will serve as interim CNO for EUHM while continuing her current roles. The search for Gullatte's replacement will begin after a new EUHM CEO is identified (anticipated in January) to replace Dane Peterson, following his appointment as EHC hospital president.
 |
Ray Schinazi (pediatrics) received the Distinguished Scientific Achievement Award from the American Liver Foundation. Read more.
 |
A clinical trial led by Steven Wolf (rehab medicine) to teach stroke patients to use their stroke-affected arm rather than their "good" arm has been identified as one of the top 15 international clinical trials ever published in physical therapy and rehab. Read more.
Event
 |
|
| Claire Pomeroy |
Nov 20: CFAR Network pizza party, featuring Claire Pomeroy, president of the Lasker Foundation, as keynote speaker: An Epidemic Without Headlines: Confronting the Crisis of HIV/AIDS in Women. 5:30 p.m., Room 1000, CNR building, RSPH. Register.
