Bridge frame will begin ascent over Haygood in early March
 |
| The steel frame (see arrow above) of the bridge that will span Haygood Drive will be lifted into place over the street during the second weekend in March. For real-time views of the construction site of the Health Sciences Research Building, see photos from webcam. |
The steel "shell" of the bridge that will connect the new Health Sciences Research Building and the Emory-Children's Center will be put into place over Haygood Drive during the weekend of March 9. The structure is 175 feet long and 35 feet wide and weighs 200,000 lbs.
Two cranes will be needed to move the bridge, and just lifting it up will take about eight hours, according to Charlie Andrews, senior AVP for space planning and construction. When completed, the bridge will do more than connect two buildings. It will be a working bridge, with research offices and "dry" research space.
Placing the bridge frame above the street will necessitate the closure of Haygood Drive from Andrews Circle (at Druid Hills High School) to Clifton Road. The road will be closed during these times:
• 7 p.m., Friday, March 9 to 6 a.m., Monday, March 12
• 7 p.m., Friday, March 23 to 5 a.m., Monday March 26
 |
| The bridge as it will look when completed, viewed from the southeast. |
During the weekend of March 23, workers will build a steel platform on which to stand to continue bridge construction, which is expected to last six months.
Access to Druid Hills High School and to the Lowergate and Tower parking decks will not be affected. Emory shuttle service also will not be affected.
Drivers should expect periodic one-lane road closures on Haygood Drive after 7 p.m. from March 9 to April 9.
The Health Sciences Research Building is expected to be completed in April 2013.
EUH ED to be renovated for increasing patient volume
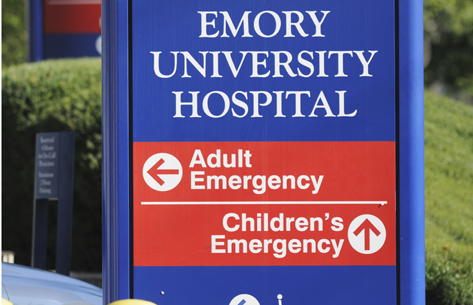 |
| The emergency department at Emory University Hospital will double in size when renovation is completed. |
Walk into any hospital emergency department (ED) during peak hours and you are likely to find people waiting while physicians and nurses address first the most urgent cases. The ED at Emory University Hospital (EUH) is no different.
 |
|
| Matt Keadey |
|
 |
|
| Kate Heilpern |
|
When ED physician Matthew Keadey arrived at EUH in 2000, he and his colleagues saw approximately 15,000 patients annually. Today, they see 36,000, and in just three years, they expect that number to climb to 44,000—all in
an ED space that was never meant to be an ED. (Up until 1998, EUH didn't have an official ED.)
"I liken our space to a hermit crab," says Keadey. "We had a shell, and we backed into it."
Keadey, though, is pleased that relief is in sight. EUH will begin renovation of its ED in August, taking the current 9,600-sq.-ft. space to 19,000 sq. ft. The number of exam rooms will increase from 21 to 32, and all will be private rooms. Most of them will be 144 sq. ft. with a standard design, so health care providers can find supplies in the same place in each room.
Space will be better designed, Keadey says, with patient rooms located in the line of sight of the nursing station. (The current "shotgun house" style has patient rooms off of a long hallway.) Non-ED foot traffic will be reduced, with the establishment of a separate ED entrance. The waiting room will be expanded, and the intake area will be more private.
The ED also will gain imaging capabilities (X-ray and CT scan), valuable time-savers considering EUH's patient population, says Kate Heilpern, chair of the Department of Emergency Medicine in the medical school.
The average ED in the United States admits 12% of its patients. Emory University Hospital's ED admits 38% because it receives some of the area's sickest patients.
"The volume in every ED is growing," says Heilpern, "but we have a more complex patient population at Emory University Hospital that generally requires more time, more advanced imaging studies, and more laboratory studies to conduct an evaluation."
 |
| The existing layout of Emory University Hospital's emergency department. |
To give the ED more room, 5,700 sq. ft. of lab space will be moved to
basement level. The current occupants of the basement—risk management, employee health, and security—will move to the second floor, after patient financial services moves to the Emory Healthcare North Decatur office this month.
Plain-speak about the economy and health care
Our national debt and the cost of health care will increase sharply over the next 10 years if we maintain status quo, says Steven Lipstein, CEO of BJC Healthcare in St. Louis.
Lipstein gave his outlook on the economy and health care reform at Emory on Jan. 31 as part of Woodruff Health Sciences Center's Future Makers lecture series. Lipstein, who received his undergraduate degree from Emory in economics in 1978, oversees 13 hospitals, including two teaching hospitals affiliated with Washington University. Lipstein also chairs the board of directors of the St. Louis Federal Reserve Bank and is vice chair of the board of the Patient-Centered Outcomes Research Institute (PCORI), established under the Patient Protection and Affordable Care Act.
| |
 |
| |
Steven Lipstein |
Lipstein put the current financial crisis in historical perspective. "We've been in a worse fiscal situation than today," he said. Paying debt from the Civil War took 50 years, and we didn't pay off World War II till about 1970. Paying down the current debt will take a long time as well.
One of the first steps toward this goal is to change the current ratio of debt to gross domestic product (GDP). To be sustainable, national debt, currently at 100% of GDP and rising, needs to be at a constant or declining ratio of no more than 60% of GDP, he explained. To achieve this 60% ratio in 10 years, cuts of $4 trillion are needed—a consensus figure agreed on by members of both political parties.
In terms of where health care fits into the equation for the escalating debt-to-GDP ratio, Lipstein blamed some of the current financial difficulties not on Republicans or Democrats but on increasing life expectancy, which was only 72 years when Medicare was created in 1965. Medicare currently can afford to provide coverage only about 15 years beyond age 65. Meanwhile, the current 47 million total of Medicare enrollees is expected to grow to 70 million in the coming years.
In terms of how U.S. health care expenditures compare with those of other developed countries, Lipstein also lent an economist's perspective. We spend more, he explained, because our per capita costs are higher. They are higher because a higher percentage of the population lives in poverty (15%), compared with the average for developed nations (10%). While we deal with the symptoms of high costs, is part of the underlying cause really poverty, he asked.
Whatever the symptoms and causes, the fact remains that health care will have to adapt as efforts are implemented to achieve a sustainable debt-to-GDP ratio over the next decade. We will need to reduce hospital readmission rates, said Lipstein, rely more on multi-disciplinary teams to manage chronic disease, increase the number of ambulatory care facilities, and accelerate comparative effectiveness research. If we don't do this, he said, insurance companies will do it for us, and they will use claims data rather than patient-centered data to reduce payments and utilization.
Lipstein believes that comparative effectiveness research, which PCORI was created to help fund and implement, has great potential for lowering costs and increasing quality. PCORI has earmarked $3 billion for research grants through 2019 and expects to make its first funding announcements in May. "We hope Emory will be a major applicant for funding," he said. [Editor's note: Researchers in health sciences submitted a total of 10 applications for the first round of PCORI grants.]
While he was here, Lipstein also spoke at a Health Innovation Program (HIP) symposium, the first in a quarterly HIP series on fixing what's broken in health care.
Building consensus and getting the best value
| |
 |
| |
Rosemary Linacre |
| |
|
One in a series of profiles of people in the Woodruff Health Sciences Center
In her first big project after becoming Emory Healthcare's first value analysis director in 1997, Rosemary Linacre got something of a rude awakening.
She was charged with replacing all IV pumps across the system. The task sounded straightforward enough (after all, the new pumps were better, and the existing ones were no longer even being made), but it proved surprisingly complicated.
Linacre, a former surgical services nurse, encountered keen resistance from nursing staff who had relied for years on those pumps and the practice methods that went with them. "I sometimes felt as if I were ripping a child from its mother's arms," she remembers.
She learned quickly, however, and by the end of the changeover, she had earned everyone's trust with implementation of a highly inclusive and objective decision-making system still in use today.
The goal of value analysis is to keep track of new products on the market, decide what is best for quality of care, add needed good products, reduce or eliminate less useful ones, standardize equipment (and thus training) across Emory Healthcare, and get the most possible value for dollars spent.
An interdisciplinary committee for product value analysis established by Linacre 12 years ago is key to those goals and to the acceptance and smooth implementation of new or upgraded products. Gone are the days when a single physician could decide to change a product. Today, the committee has representatives from all areas affected by new products—especially front-line, hands-on users like clinical nurse specialists and physicians—and from related sources of expertise such as infection control, pharmacy, quality, radiology, anesthesiology, and biomedical engineering. In fact, 30 to 40 members attend each monthly meeting, listening to pitches by vendors first screened by Linacre, comparing products, studying spreadsheets, and making recommendations about changes.
In addition to the committee she leads, Linacre benefits from expertise provided through the University HealthSystem Consortium, through which she received training in value analysis when this area first originated as a new profession in health care in the 1990s.
Today, Linacre once again finds herself involved in implementation of new IV pumps, this time, "smart" wireless devices loaded with fail-safe alarms, soft stops that ask if you are sure this is the right dose, and hard stops that simply say no. The new pumps are already in place and training is completed at Emory University Hospital and EU Orthopaedics & Spine Hospital, with Emory Midtown and Wesley Woods next in line. When complete, the changeover, including training, will have taken less than a year, and no one thus far, including Linacre, has shed any tears.
|
|
 |
|
From the Executive VP
 |
| Wright Caughman |
|
State of the WHSC
Thanks to those of you who were able to attend the annual State of the Woodruff Health Sciences Center address earlier this week. I'll also be visiting Emory University Hospital Midtown (February 23) and Grady (February 29) to deliver the address, and I hope you'll be able to join me for one of those dates if you couldn't make it to WHSCAB. If not, we've posted video of some of the highlights of this week's event. Please click on the links below to view them. You can also click below to download a year-in-review slide deck showcasing many—though by no means all—of our terrific accomplishments over the past year.
View video and slides.
What really distinguishes the Woodruff Health Sciences Center is that we are an essential part of a university community and mission—one that strives not only to understand the human condition, but to improve it through education, discovery, and service. Thanks to our extraordinary faculty, staff, students, and supporters, we are leading positive transformation in the world and having a meaningful impact on the lives of others.
As always, thanks for all that you do to move our important work forward.
Please let me know your thoughts and suggestions at (evphafeedback@emory.edu)
In brief
New Emory Healthcare advertising campaigns
 |
| TV commercial for EUOSH |
|
Emory Healthcare recently launched new advertising campaigns for Emory University Orthopaedics & Spine Hospital (EUOSH) and Emory Johns Creek Hospital. The EUOSH campaign is running on radio and TV through April. The campaign celebrates the hospital's high patient-satisfaction scores. Check out the TV spot, which features many of the hard-working staff at EUOSH. Emory Johns Creek Hospital's first TV advertising campaign will run through June on targeted cable stations broadcasting in and around the Johns Creek area. This TV spot's goal is to showcase the variety of services offered by the hospital to the community.
Emory Vaccine Center paper honored by vaccine society
 |
| Bali Pulendran |
|
A research paper by Emory Vaccine Center scientists was honored as the 2011 Paper the Year by the International Society for Vaccines. The paper, "Systems biology of vaccination for seasonal influenza in humans" was published in Nature in July. The senior author was Bali Pulendran, and Jens Wrammert and Rafi Ahmed were co-authors. The society called the paper a "landmark study" that "highlights one of the ways for the future of vaccinology."
Emory Healthcare connects with Delta
 |
|
| Susana Alfonso |
|
Emory Healthcare has partnered with Delta Airlines on the new Emory Clinic at Delta. The clinic is connected to a Walmart pharmacy and store and provides full primary care to all Delta employees and their dependents, retirees, and contractors, approximately 30,000 people in metro Atlanta. Susana Alfonso, a general practitioner, is the primary physician at the clinic.
"This is bringing an integrated health care system to where the patients are,"
she says.
Notable
 |
| Tim Buchman |
|
Tim Buchman, director of Emory's Center for Critical Care, will be inducted into the Johns Hopkins Society of Scholars in April. The society was established in 1967 to honor distinguished former Johns Hopkins postdoctoral fellows and junior or visiting faculty. Buchman was also one of 20 physicians to be named among the American College of Critical Care Medicine's first class of Master of Critical Care Medicine Fellows during the Society of Critical Care Medicine's 41st congress earlier this month in Houston. Read more.
 |
| Walter Curran |
|
Walter Curran, executive director of Winship Cancer Institute, is number 22 among 35,000 researchers nationwide in a survey of National Institutes of Health grant funding. Curran, whose NIH research funding totaled $16,074,557 last year, is the only researcher in Georgia and the only NCI-designated cancer center director to be among the top 25 in NIH grant funding.
 |
| Gary Miller |
|
Gary Miller has been named a 2012 Distinguished Investigator by the Georgia Research Alliance. The designation includes a $500,000 award over five years. Miller is associate dean for research at Rollins School of Public Health and directs the Emory Parkinson’s Disease Collaborative Research Center. Read more.
 |
|
| Ignacio Sanz |
|
Ignacio Sanz has been named a Georgia Research Alliance Eminent Scholar and director of Emory's Kathleen and Mason Lowance Center for Human Immunology. He is coming to Emory from University of Rochester and will join the departments of medicine and pediatrics April 1. His expertise is in autoimmune B-cell diseases with a special focus on systemic lupus erythematosus. Sanz also will direct the Division of Rheumatology in the Department of Medicine and will hold the Mason Lowance Chair in Human Immunology. Read more.
Events
 |
|
| Phinizy Calhoun Sr. |
|
Feb 17: Re-dedication of the Calhoun Oak, lawn of Emory University Hospital, 2 p.m. (Original oak removed last year because of ambrosia beetle infestation.) The tree is named for the late ophthalmologist Phinizy Calhoun Sr, who donated funds to establish Emory's Health Sciences Library in honor of his father, A.W. Calhoun, and grandfather, A.B. Calhoun. The latter helped found the medical school's antecedent school, Atlanta Medical College, in 1854. Phinizy's son, Phinizy Calhoun Jr., performed Emory's first cornea transplant in 1947. Read more about the Calhouns' contributions to Emory.
Feb. 18: Spin to End AIDS 2012, to benefit the Emory Vaccine Center, 6 p.m., Athletic Club Northeast. More info.
Through Feb. 29: Two National Library of Medicine exhibits at the Woodruff Health Sciences Library, Changing the face of medicine: Celebrating America's women physicians and Binding wounds, pushing boundaries: African Americans in Civil War medicine.
March 8: 6th Annual Celebration of Technology and Innovation by the Emory Office of Technology Transfer, 5 p.m., Emory Conference Center. To RSVP contact Ashley Myers.
April 2: 4th Annual Georgia Nanotechnology & Infectious Disease Symposium, 8:30 a.m., WHSCAB auditorium. More info.
|

