





|
 |
| |
|
|
| |
 E-mail
to a Friend
E-mail
to a Friend  Printer
Friendly Printer
Friendly |
|
| |
|
|
| |
In
June 1981, a CDC report described a cluster of previously healthy
homosexual men from Los Angeles who had contracted Pneumocystis
carinii pneumonia (PCP). Two of the five men treated for this
rare form of pneumonia had died.
James Curran, dean of the Rollins
School of Public Health (RSPH), remembers the cases clearly. Then
an epidemiologist with the CDC, he chaired the task force organized
to investigate the outbreak. Within three weeks, Curran's group
confirmed more than 25 additional cases of PCP and other serious
opportunistic infections among homosexual men in Los Angeles and
New York City. In addition, the agency reported several cases of
Kaposi's sarcoma (KS), a rare form of cancer, among gay men in New
York. The subsequent case definition for disease surveillance put
in place by Curran and colleagues at the CDC was adopted worldwide,
allowing early and consistent recognition of a new global epidemic.
What experts detected was AIDS, short
for acquired immune deficiency syndrome, so named by the CDC task
force in 1982. For the past quarter century, Curran and others around
the world have made it their mission to halt transmission of the
disease and find a cure. Here, he looks at the past, present, and
future of HIV/AIDS. |
|
| |
|
|
| |
Q.
Why did the first cases of PCP and KS attract
your attention?
A. Prior to these cases, CDC epidemiologists had investigated a
variety of new outbreaks, including toxic shock syndrome, Legionnaire's
disease, and swine flu. When the first cases of PCP were reported,
many of us who had worked with gay men in studies of hepatitis or
sexually transmitted diseases knew quickly it was an important problem
that deserved focused and immediate attention.
These cases were important because
previously healthy people were dying of an unexplained disease.
It was clustered among gay men, it was fatal, and the cause was
unclear. We needed to find out was it new? Was it restricted to
Los Angeles and New York? Was it restricted to gay men? Was it increasing?
And what was the extent of the problem?
Q. How did you and the CDC confront this problem?
A. The first step in understanding this apparently new epidemic
was to develop a case definition and conduct intensive surveillance
for cases of Kaposi's sarcoma and opportunistic infections, which
we later termed as AIDS. The case definition was intended—and
subsequently proven—to be highly specific. This definition
was rapidly adopted worldwide. It allowed for precise and consistent
identification of epidemiologic patterns in the United States and
other parts of the world with sophisticated health care. |
|
| |
|
|
| |
|
|
| |
|
|
| |
Q.
How did the disease come to be named AIDS?
A. After a year or so, we felt a need to pull together the collections
of opportunistic cancers and other conditions under a name that
could replace the various terms being used—Kaposi's sarcoma,
opportunistic infections, GRID
or gay-related immune deficiency. The CDC started to use the name
AIDS—acquired immune deficiency syndrome—to best describe
the underlying problem that ultimately was found to be caused by
HIV (human immunodeficiency virus) in 1983.
Q. How did HIV/AIDS evolve?
A. The period between 1981 and 1986 was a time of tremendous discovery.
During the first two years, modes of transmission were defined.
Scientists confirmed the disease among gay men, intravenous drug
users, and their sexual partners. They also investigated three cases
of PCP among men with severe hemophilia A and no other known risk
factors. The identification of these and other people with hemophilia
provided solid epidemiologic evidence that a blood-borne and sexually
transmitted pathogen caused AIDS. Completing the picture, investigators
confirmed AIDS was transmitted from mother to child and through
heterosexual contact. The CDC took important steps to protect health
care workers and blood supplies and to educate the public about
transmission and prevention. In 1983, investigators at the Institute
Pasteur in France identified HIV as the virus that causes AIDS.
In 1984, the diagnostic test to detect HIV in the blood became available.
By 1986, Dr. Meade Morgan, a colleague at the CDC and an eminent
RSPH alumnus, predicted a total of 270,000 AIDS cases through 1991,
thus forecasting enormous morbidity, mortality, and health care
costs for the nation in the ensuing years. |
|
| |
|
|
| |
 |
|
| |
|
|
| |
Q.
During this time, you led the CDC's effort to formulate recommendations
to protect the nation's blood supply. What was the result?
A. In early 1983, before the discovery of HIV, the CDC and the U.S.
Public Health Service recommended that persons at increased risk
for AIDS not donate blood. Testing the blood supply was a breakthrough.
There were relatively few tests for infectious diseases that were
implemented before the AIDS era. Now there are more than a dozen
tests to protect the blood supply. This was because of a tremendous
effort to eliminate infectious diseases from blood.
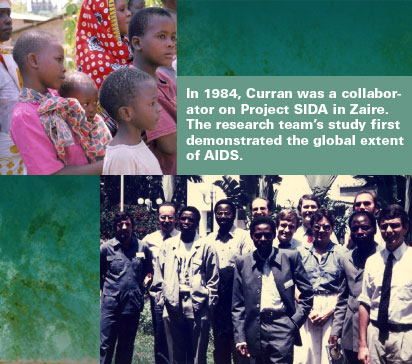
Q. When did the global extent of AIDS first become known?
A. Data collected by researchers at Project SIDA in Zaire demonstrated
an extensive epidemic there in 1984. It was the highest estimated
HIV infection rate in the world at the time. This year, the Joint
United Nations Program on HIV/AIDS reported more than 25 million
deaths by the end of 2005 and nearly 40 million people infected
worldwide. With nearly 3 million deaths in 2005, HIV/AIDS is now
the fourth leading cause of death in the world. With 4.1 million
new infections in 2005, deaths will likely continue to rise.
Q. When did the first drug therapies for AIDS become available?
How did they progress?
A. In 1987, AZT (azidothymidine) was licensed as the first antiretroviral
drug to treat HIV. In the 1990s, the biggest news concerned two
discoveries. First was that providing AZT to HIV-infected women
during pregnancy could reduce the risk of transmission to newborns.
The second was the availability of highly active antiretroviral
therapy or HAART. This therapy, which combines at least three drugs,
has greatly prolonged lives and improved the well-being of millions
of people throughout the world. Antiretroviral drugs were discovered
by a variety of people, mostly in this country, and Emory has played
a major role in their development. Two of the major drugs—3TC
and FTC—were invented here by researchers Dennis Liotta and
Raymond Schinazi. |
|
| |
|
|
| |
|
|
| |
|
|
| |
Q.
At the time of these discoveries, you observed a sense of complacency
about HIV/AIDS. Why?
A. In the early 1990s, a sense of complacency emerged, particularly
in the United States and developed countries, when the number of
HIV/AIDS cases began to level off. There was a feeling that the
horizons were clear and that people could understand who was at
risk and who wasn't. The general population began to implicitly
accept the current number of cases.
Q. How do you combat that sense of complacency?
A. We all exist in a social, cultural, and economic context. We
also live at a certain level of health and a certain level of public
health. But there are great differences in the health of some populations
and in the health of some countries. When a new epidemic or disease
comes along, we are tempted to say, "Oh my goodness, we've
become such an obese country. Oh my goodness, we have 40 million
cases of AIDS throughout the world. That's just the way things are.
We'll just have to accept that." Improving the health of a
population or country requires looking for ways to redefine the
unacceptable and rise above the status quo.
Q. How do you maintain commitment to HIV prevention?
A. It's important to realize that 4 million people are having sex
for the first time each year in the United States and that education
and prevention efforts must continue. We can't sit back and say,
"Well, we did comprehensive sex education 10 years ago. Why
do we need to do it now?" There's a need for constant renewal
of information to go along with the renewal of potential risk.
Q. From the beginning, HIV/AIDS has been a source of social
controversy. At one point, protesters spit on you, and your face
appeared on 20,000 postcards sent out by activists. How did you
react to that?
A. I, Tony Fauci of the NIH, and others from the CDC were speaking
at a public engagement when we were targeted. Many government scientists
were seen as representatives of the U.S. government as a whole.
To some extent, you have to take that kind of protest and figure
out the meaning of it and not take it personally. Is it legitimate?
Why is it being conducted? Is there truth in what they say?
|
|
| |
|
|
| |
 |
|
| |
|
|
| |
Q.
Was there truth in what they were saying?
A. There was an enormous amount of impatience regarding the government's
response to AIDS. People were dying. The diagnosis of HIV or AIDS
was a death sentence, so they were impatient to help find more effective
therapies. And they were mistrustful of government, particularly
homosexual men and women and injecting drug users who felt their
behavior, and sometimes their very existence, was seen as criminal
by some people.
Q. What lessons from HIV/AIDS can be applied to other diseases?
A. There were lessons to be learned from tracking and combatting
the disease and working with communities and the social environment.
There were advantages in the discovery of drugs to combat it. For
example, 3TC, which was invented here at Emory, is also effective
against the hepatitis B virus. The social activism of the 1980s,
which brought public and private attention to AIDS as a health problem
and as a public health problem, has been shown to be effective for
cancer and other diseases. |
|
| |
|
|
| |
|
|
| |
|
|
| |
Q.
In 1995, you left the CDC to become dean of the RSPH. What was the
HIV/AIDS research culture like at Emory?
A. There were a number of investigators working on HIV/AIDS across
Emory. Most of their work was domestic. There was little work globally.
David Stephens, director of the Division of Infectious Diseases
in the School of Medicine, and I formed an AIDS interest group.
From there came a desire to grow and coordinate AIDS research more
effectively and to recruit more expert faculty. In 1997, the RSPH,
the School of Medicine, and the Yerkes National Primate Research
Center formed the Emory Center for AIDS Research (CFAR), with funding
coming from the NIH a year later.
Q. What has CFAR enabled Emory to do?
A. Emory is one of 21 federally funded Centers for AIDS Research
in the United States. Our center is unusually broad in its vision
and initiatives. Prevention is a central theme—health education,
research on preventing transmission among adolescents, developing
and testing of HIV vaccines, testing microbicides, and prevention
and treatment of antiretroviral infections and tuberculosis to prevent
complications from these diseases. We work with colleagues in Atlanta,
throughout the United States, and in several developing countries,
including Rwanda, Zambia, South Africa, Ethiopia, and India. Emory
doctors care for 6,000 to 7,000 patients annually. That's one of
the largest HIV/AIDS patient groups in the country. |
|
| |
|
|
| |
| |
|
|
| |
A
Research Powerhouse |
|
| |
By
pooling resources and expertise, the Emory Center for
AIDS Research (CFAR) has become a powerhouse in the
global quest to help individuals, families, and populations
affected by HIV/AIDS. Since its startup in 1997, funding
for HIV/AIDS research has more than tripled to $55 million
a year. Currently, 163
studies are under way.
Essentially, the Emory
CFAR is a giant umbrella encompassing the RSPH, where
the center is housed; the School of Medicine; Yerkes
National Primate Research Center; the Emory Vaccine
Center and the Hope Clinic for vaccine and microbicide
testing; Emory Crawford Long Hospital; the Ponce de
Leon Center, a highly regarded outpatient HIV/AIDS clinic
operated by the Grady Health System; and the Atlanta
Veterans Affairs Medical Center.
More than 100 Emory faculty
members are engaged in CFAR through collaborations in
behavioral and social science, medicine, nursing, statistics,
virology, pharmacology, and immunology and through partnerships
with government agencies, private AIDS researchers and
clinicians, and other universities. Several service
cores spread across campus support their research in
prevention science, vaccine development, AIDS pathogenesis,
and clinical science. Three of those units—the
Biostatistics Core, directed by Michael Kutner; the
Social and Behavioral Sciences Core, directed by Gina
Wingood; and the Administrative Core—are in the
RSPH.
CFAR faculty stay attuned
through a website and through the Vaccine Dinner Club
and the CFAR AIDS Soiree, successful programs featuring
prominent speakers. Just as important, CFAR provides
funding to help junior faculty jump-start their research
programs and to recruit key investigators.
Three co-directors lead
the center. James Curran, dean of the RSPH, serves as
CFAR's principal investigator. Carlos del Rio (below
left), an expert on HIV/AIDS in developing countries,
treats patients at Grady Memorial Hospital and the Ponce
Center. Eric Hunter (below right), a Georgia Research
Alliance Eminent Scholar, is among the world's leading
experts on retroviruses and maintains a laboratory at
Yerkes.
To learn more about CFAR,
visit the new website at www.cfar.emory.edu.

|
|
|
|
|
| |
|
|
| |
|
|
| |
Q.
What is CFAR's greatest accomplishment to date?
A. CFAR crosses schools and centers to create a multidisciplinary
research environment. We now have three directors—myself and
Carlos del Rio and Eric Hunter, who are both in the School of Medicine.
We bring complementary talents, interests, and geographic settings
to the endeavor. There's a huge difference in awareness, capacity,
and accomplishments among AIDS researchers at Emory compared to
nine years ago. We have an active group of more than 100 faculty
who are really making a difference. In the past nine years, funding
for AIDS research at Emory has more than tripled to $55 million
per year.
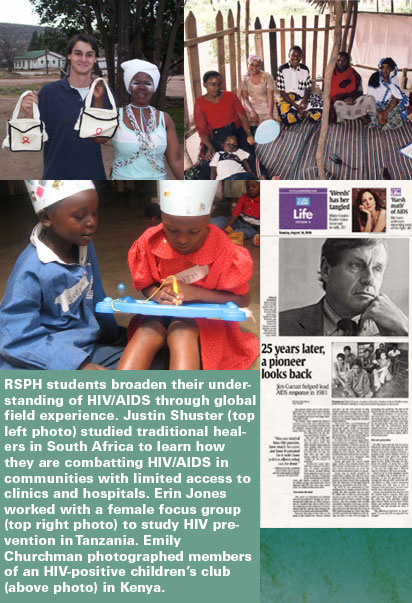
Q. What comes to mind when you think of the face of HIV/AIDS?
A. Many times in public health, we categorize health in terms of
numbers, economic impact, social impact. We talk about rankings
in terms of deaths, increasing numbers of cases, decreasing numbers
of cases. But the true impact of the problem affects individuals.
They are people who suffer and die,
often needlessly. They are people who survive and overcome enormous
difficulties to become the beneficiaries of science and care and
who become leaders in their own right.
They are people who work on the problem.
People who study it. People who volunteer with organizations. Young
graduate students who are inspired to go into public health because
of concerns about AIDS or people they know with the infection. Generations
of people who often take their passion and mission in life from
their experiences or concerns about friends or citizens. They are
scientists, doctors, nurses, public health workers, and policymakers
who willingly use their time, social capital, and influence to deal
with the problem. All of these individuals have a personal stake
in HIV/AIDS. |
|
| |
|
|
| |
 |
|
| |
|
|
| |
Q.
What lies ahead for people with HIV/AIDS?
A. The next 25 years of HIV/AIDS will go by in a heartbeat, just
like the first 25 years. The high rates of infection in sub-Saharan
Africa will level off through intervention and a growing capacity
among people to speak frankly about risks, stigma, and HIV counseling.
HIV/AIDS tends to settle in places where poverty is greatest and
where resources are often diverted to other problems. It's still
on the rise in China and has become a substantial problem in India
and Eastern Europe. Ultimately, HIV/AIDS will remain a huge public
health problem, barring the availability of creative therapies and
a vaccine. We need both.
I'm optimistic they will become available
and the world will find a way to use them. In the absence of that,
prevention is vital for a world where people, communities, and nations
can talk openly and comfortably about sexuality and the stigma of
HIV/AIDS. |
|
| |
|
|
| |
|
|
|
|
|
|