|
 |
|
|





|

|
|
|
| |
 E-mail to a Friend
E-mail to a Friend
 Printer Friendly
Printer Friendly |
|
| |
|
|
|
 |
Highlights:
|
 |
 |
 |
When
emergencies have to wait
Mission possible
A verdict for the common good
Protein pieces of the Parkinson's puzzle
Home
is where the transplant is
Labor of love
The
RUTH effect
Three
strikes
We've
come a long way baby
First sight
Racing for life
Milestones |
 |
 |
 |
| |
|
|
 |
| |
|
|
 |
When
emergencies have to wait
Arthur
Kellermann, Emory’s chair of emergency medicine, has watched
emergency departments (EDs) become stretched more thinly year after
year. On any given night, emergency services at Grady and
Emory hospitals reflect the typical problems of emergency rooms
across the country—overcrowding with long wait times, frequent
diversion of ambulances, and resources stretched to the max. In
the United States, ambulances are turned away from emergency departments
on average once every minute, and patients in many areas of the
country may wait long hours or even days for a hospital bed.
For more than a decade, Kellermann
has been an outspoken proponent for improving emergency medical
care, and over the past three years, he has served on a committee
of the Institute of Medicine (IOM) investigating the future of emergency
care in the United States. The committee’s final reports delivered
a devastating verdict and an urgent call to action. In short, the
emergency medical system is (in the words of the committee) “at
the breaking point”—barely able to handle daily caseloads,
much less a surge of casualties from a disaster.
“If we are struggling to deal
with tonight’s 911 calls in city after city across the United
States, how in the world are we supposed to handle an epidemic of
pandemic flu or a major terrorist attack or the next natural disaster?”
Kellermann asked a National Public Radio reporter upon release of
the reports in June.
The critical condition of today’s
emergency medical system stems from insufficient funding and steady
growth in uncompensated emergency care, according to the IOM. In
the early 1980s, federal funds for enhancing emergency response
services declined abruptly, leading to haphazard development of
EMS services. In 1986, Congress passed a law that made emergency
care a right for everyone in the United States, but it provided
no mechanism to pay for this care. Over the next 20 years, patient
volumes increased while hundreds of emergency departments closed.
In 2003, EDs received nearly 114 million patients—a 26% increase
over the previous decade—but the country lost 703 hospitals
and 425 emergency departments during the same period. Despite these
challenges, emergency medical services received only 4% of funding
distributed by the U.S. Department of Homeland Security for emergency
preparedness in 2002 and 2003.
Compounding the problem are the 45
million people in the United States who lack health insurance. Many
who are turned away from other clinical settings because of inability
to pay end up in the emergency room. Another IOM committee on which Kellermann served
calculated that U.S. hospitals and doctors lose billions annually
in uncompensated care of the uninsured, which in turn creates enormous
stress on the health care system. In the 2004 fiscal year, uncompensated
care provided by Emory physicians at Grady totaled $22 million.
(Emory Healthcare provided $51.7 million that year
emergency room. Another IOM committee on which Kellermann served
calculated that U.S. hospitals and doctors lose billions annually
in uncompensated care of the uninsured, which in turn creates enormous
stress on the health care system. In the 2004 fiscal year, uncompensated
care provided by Emory physicians at Grady totaled $22 million.
(Emory Healthcare provided $51.7 million that year
in charity care and $66 million in 2005.)
When hospitals are full, as is increasingly
the case, admitted patients often back up in the ED. When EDs become
dangerously overcrowded, the staff may ask inbound ambulances to
divert to other facilities. In 2003, U.S. hospitals diverted more
than 500,000 ambulances because of overcrowding in the ED. Diverting
ambulance patients from one hospital to another puts additional
stress on patients, family members, and the community, Kellermann
says. And when other hospitals go on ambulance diversion as well,
a community can experience the health care equivalent of a “rolling
blackout.”
Conditions in the Grady ED, which
handles more than 100,000 visits each year, reached a record low
in 2002 and 2003 when, because of crowding, average throughput times
exceeded seven hours and the ED was on diversionary status more
than 20% of the time. To counter those trends, Leon Haley, vice
chair and chief of emergency medicine at Grady, implemented a model
to identify major bottlenecks in patient flow, instituted new diagnostic
test-ordering processes, and improved staff coordination in the
ED’s fast track for people with minor illnesses or injuries.
Those efforts produced results: the ED reduced average time from
arrival to bed placement from 219 minutes to 94, a 57% decrease.
With the support of the Robert Wood
Johnson Foundation and later the Healthcare Georgia Foundation,
Haley also created an ED-based “care management unit”
with seven beds staffed by four nurses and four case managers. This
unit is used to evaluate and treat patients with chest pain, heart
failure, asthma, and hyperglycemia—conditions that would otherwise
mandate hospital admission. While these patients undergo rapid treatment,
case managers teach them how to better manage their health and arrange
follow-up with a primary care provider. The goal of the program
is to decrease the number of short-stay admissions and repeat visits
to the ED.
To promote injury prevention and public
health surveillance, Emory’s Department of Emergency Medicine
is developing programs to reduce the root causes that result in
ED visits, such as child neglect and abuse, firearm violence, and
head injuries and to improve outcomes when emergencies do occur.
Start-up support to develop innovative ideas comes from a fund created
by the Seaman family and their business, Rooms to Go. The partnership
has produced results. For example, Bryan McNally is leading Cardiac
Arrest Registry to Enhance Survival (CARES), an initiative funded
by the Centers for Disease Control and Prevention. CARES is a national
registry designed to help communities across the United States identify
when and where cardiac arrest occurs, which elements of their EMS
system are functioning properly and which are not, and what changes
are needed to improve outcomes. Emory researchers are compiling
and analyzing preliminary CARES data to drive improvements in treatment
in Fulton County, soon to be expanded to all of metro Atlanta, and
ultimately, nationwide.
In another cardiac care initiative,
Emory emergency physicians partnered with Grady and the Emory Heart
Center to improve the prehospital treatment of heart attack victims.
With the support of Medtronic/Physio-Control, Cingular Wireless,
and Nokia, Grady ambulance crews were trained and equipped to obtain
12-lead ECGs in the field and transmit them via cell phone to an
emergency physician at Emory Crawford Long hospital. If the ECG
showed signs of a major heart attack, the patient was offered the
option of direct transport to the cath lab at either Emory University
Hospital or Emory Crawford Long. The pilot program was so successful
that a consortium of Atlanta’s leading hospitals is joining
Emory to expand it throughout the metro area. The initiative will
operate under a new name, Timely Intervention in Cardiac Emergencies
(TIME). Like CARES, TIME has the potential to transform emergency
cardiac care nationwide.
From yet another tack, Emory’s
interdisciplinary emergency nurse practitioner program—offered
through its schools of Nursing and Medicine and one of only four
of its kind in the nation—is helping improve ED patient flow
by training nurse practitioners to provide cost-effective health
care in emergency settings.
According to the IOM report, innovative
solutions like these are needed to strengthen the nation’s
emergency care system. The report calls for reform of reimbursement
policies to reward hospitals that end ED boarding and stop diverting
ambulances. Penalties might be assessed for those that willfully
fail in this area.
The report also calls for a pool of
at least $50 million to reimburse hospitals for uncompensated emergency
and trauma care as well as substantial increases in federal funding
to provide hospitals with resources needed in disasters. And it
recommends the allocation of $88 million in seed grant funding over
five years for pilot projects to promote coordination and regionalization
of emergency care.
If getting the word out helps Congress
open its wallet for emergency care, then Kellermann is doing his
part. Covered in more than 172 news sources across the United States,
including NPR, CNN, the Associated Press, and USA Today, the chair
of emergency medicine may finally have a soapbox tall enough from
which to be heard.
For more details on the report, click
here.
This
fall, Kellermann is on sabbatical as a Robert Wood Johnson Health
Policy Fellow in Washington, DC.
|
 |
| |
|
|
 |
| |
|
|
|
| |
 |
Mission
possible
 The
idea is no small one: to relocate Emory University Hospital to the
east side of Clifton Road alongside a new clinic cluster for outpatient
care, medical faculty offices, and medical research. But
the Emory Board of Trustees is thinking large-scale and long-term,
and in June, it officially accepted the results of a nine-month
feasibility study. Following the recommendation of the Woodruff
Health Sciences Center board, the University’s Board of Trustees
authorized preparation of architectural schematic designs for new
hospital and outpatient facilities that could take as long as a
decade and as much as $2.2 billion to realize. The
idea is no small one: to relocate Emory University Hospital to the
east side of Clifton Road alongside a new clinic cluster for outpatient
care, medical faculty offices, and medical research. But
the Emory Board of Trustees is thinking large-scale and long-term,
and in June, it officially accepted the results of a nine-month
feasibility study. Following the recommendation of the Woodruff
Health Sciences Center board, the University’s Board of Trustees
authorized preparation of architectural schematic designs for new
hospital and outpatient facilities that could take as long as a
decade and as much as $2.2 billion to realize.
The new medical complex will enable
Emory to achieve its vision to transform health and healing in the
21st century, says Michael Johns, CEO of the Woodruff Health Sciences
Center. That vision involves integrated care centered on the patient
with an emphasis on predictive medicine. “These new facilities
will support research, patient care, and medical training in a new
and more nimble way that sets the standard for teaching hospitals
everywhere,” Johns says.
At the centerpiece of the plan is
a new 700-bed hospital that will feature underground parking, a
spacious atrium, and retail shops for the convenience of patients
and visitors. The new hospital will combine beds from the current
84-year-old Emory University Hospital facility and other Emory facilities
on Clifton Road.
However, a new hospital and clinic
are far from a done deal. Several remaining decision points in the
next few years will determine the eventual size and configuration
of the new health sciences complex. “The trustees have made
it clear that we must proceed through this process in deliberate
step-wise fashion with periodic reality checks on funding, feasibility,
and advisability,” says John Fox, CEO of Emory Healthcare.
“We will always be planning many steps ahead, but our ability
to get to the end depends on world-class execution at every stage.
Convenient and accessible transportation for our patients, doctors,
nurses, and staff will be job one, and that’s where we are
starting.”
Beginning in the summer of 2007, the
Turman Residential Center will be demolished to make way for construction
of a 720-space parking deck. That deck, which will connect by a
pedestrian tunnel to the eventual site of the new clinic and hospital,
should be available for use by the summer of 2008. The spaces will
replace parking that will be lost in the physicians and Scarborough
parking decks and in one-third of the Lowergate deck when site preparation
for the new clinic is scheduled to begin.
The hospital and clinic development
are part of a larger ambitious strategy by Emory to enhance the
livability, accessibility, and vibrancy of its campus and the surrounding
community. Goals include restoring a walkable environment, creating
a landscaped public realm, transforming Clifton and North Decatur
roads, and expanding transportation options for the area. Emory
also is making plans to develop a campus in midtown Atlanta encompassing
Emory Crawford Long Hospital.
The mission is large but not impossible.
In the words of Fox, “Over the next 10 years, we will build
an Emory that is a source of pride and hope for everyone who needs
the support of a more accessible, more navigable, and more patient-friendly
health care system.”
|
 |
| |
|
|
 |
| |
|
|
|
|
 |
A
verdict for the common good
 Support
for creating specialized health courts is growing. U.S.
Senate Majority Leader Bill Frist and the Progress Policy Institute,
known in the 1990s as President Clinton’s “idea mill,”
have endorsed the concept. So have more than 80 leaders in U.S.
health care, including Woodruff Health Sciences Center CEO Michael
Johns, and a broad coalition of patient advocates and health care
providers, including Emory Healthcare. Known as Common Good, the
bipartisan legal reform group is championing such courts as a way
to restore reliability to medical justice. Support
for creating specialized health courts is growing. U.S.
Senate Majority Leader Bill Frist and the Progress Policy Institute,
known in the 1990s as President Clinton’s “idea mill,”
have endorsed the concept. So have more than 80 leaders in U.S.
health care, including Woodruff Health Sciences Center CEO Michael
Johns, and a broad coalition of patient advocates and health care
providers, including Emory Healthcare. Known as Common Good, the
bipartisan legal reform group is championing such courts as a way
to restore reliability to medical justice.
These health courts would be devoted
exclusively to addressing health care issues, just as existing specialized
courts already focus on taxes or drugs, for example. The hallmark
of the courts would be full-time judges with training in health
care issues, enabling them to define and interpret standards of
care in malpractice cases. Other key features of the courts would
include neutral experts, efficient proceedings to reduce attorney’s
fees and administrative costs, and predictable damages with compensation
for pain and suffering set by a predetermined schedule. State policy
makers would decide jurisdiction and selection of judges.
Six health systems have signed on
to express a strong interest in participating in a pilot project
to set up such courts. In addition to Emory Healthcare, they are
Duke, Jackson Health System at the University of Miami, Johns Hopkins,
New York-Presbyterian, and Yale. Common Good is leading the effort
in partnership with the Harvard School of Public Health and funding
from the Robert Wood Johnson Foundation.
At press time, senators had introduced
a bill to establish pilot courts. To follow the progress, see www.cgood.org.
|
 |
| |
|
|
 |
| |
|
|
|
|
| |
|
|
|
|
|
|
 |
Protien pieces of the Parkinson's puzzle
Emory scientists are making advances in uncovering the mysterious
function of the protein DJ-1. The ultimate goal for the search?
To find potential cures for nonhereditary Parkinson’s disease
and other neurologic degenerative disorders, such as Alzheimer’s.
The function of the DJ-1 protein is
unknown, but what scientists do know is that abnormalities in DJ-1
directly cause hereditary (familial) Parkinson’s disease.
Approximately 10% of Parkinson’s cases are hereditary forms
caused by a deletion of a gene or mutations resulting from substitutions
of amino acids.
But what causes the other 90% of cases
that are uninfluenced by genetics? Pharmacologist Lian Li
wondered if DJ-1 mutations play a role in nonhereditary (sporadic)
Parkinson’s, too. In research funded by the National Institutes
of Health, she has discovered that DJ-1 in patients with sporadic
Parkinson’s showed signs of oxidative stress, an imbalance
of antioxidants (agents that prevent oxygen from combining with other substances) and pro-oxidants in cells. The
damage included structural changes as the protein accumulated additional
oxygen molecules.
combining with other substances) and pro-oxidants in cells. The
damage included structural changes as the protein accumulated additional
oxygen molecules.
In essence, this imbalance results
in an excess of reactive oxygen species (harmful oxygen-containing
molecules that can cause damage to proteins). These modifications
to DJ-1 caused by the oxidative stress are irreversible and irreparable.
As with familial Parkinson’s disease, structural changes to
the DJ-1 protein in sporadic Parkinson’s signal an abnormality,
leading to eventual degrading and loss of the protein.
“The protein unfolds and cannot
function normally,” Li says. “Not recognizing the unfamiliar
shape of the protein, the cell breaks it down. The end result is
the same: you lose your protein. Any mutation or modification causing
this protein to lose its function will then lead to neurodegeneration
seen in Parkinson’s disease.”
Li and her team are now building on
the research, published in the April 21 issue of the Journal
of Biological Chemistry, to better understand the role of DJ-1.
Based on biochemical analysis, Li believes that DJ-1 may serve as
a protease, a protein-splitting enzyme that activates and deactivates
a protein by cleaving the bonds that connect its amino acids. If
DJ-1 serves as an antioxidant, then the cell may be left unprotected
when they protein is mutated or damaged.
Results of Li’s study
may lead scientists to develop drugs to target DJ-1, thereby stopping
or reversing Parkinson’s or Alzheimer’s diseases. In
the meantime, Li suggests alternative health approaches such as
the antioxidants found in green tea or vitamin C supplements as
prevention measures. |
 |
| |
|
|
 |
|
| |
| |
| |
|
|
|
|
|
|
 |
Home
is where the transplant is
In
June, the Mason Outpatient Transplant Clinic dedicated a comprehensive,
state-of-the-art clinical and patient education center in Emory
Clinic, more than tripling its former size. The new clinic,
funded by a $1.8 million grant from the Carlos and Marguerite Mason
Trust, features a waiting room that seats more than 80, computer and Internet access for patients, education
classrooms, evaluation suites with multi-media capability, 20 exam
rooms, increased infusion room capacity, advanced biopsy procedure
rooms with high-tech ultrasound equipment, and expanded clinical
lab space.
than 80, computer and Internet access for patients, education
classrooms, evaluation suites with multi-media capability, 20 exam
rooms, increased infusion room capacity, advanced biopsy procedure
rooms with high-tech ultrasound equipment, and expanded clinical
lab space.
“In the early years of transplantation,
the focus was simply to get a surgeon and an organ to save a life,
but this is too narrow a perspective,” says Christian Larsen,
Carlos and Marguerite Mason Professor of Surgery and director of
the Emory Transplant Center. “To truly restore life and health
for the whole person requires a team of physicians, surgeons, nurses,
social workers, infectious disease specialists, psychiatrists, and
dermatologists—matched with an administrative team, financial
coordinators, and more. This clinic gives those teams a home.”
Michael Johns, CEO of the Woodruff
Health Sciences Center, describes the Emory Transplant Center as
“a model of the integrated, patient-center research and clinical
care we are pioneering and perfecting at Emory. Transplantation
is one of the first investments the health sciences center is making
to truly enable the transformation of health and healing.”
In 2005, the Mason Transplant Outpatient
Clinic had more than 17,000 patient visits, including 7,000 lab
visits, 400 infusions, and 10,000 provider visits. With the increased
capacity, the clinic projects more than 20,000 patient visits in
2006 and more than 23,000 in 2007. |
 |
| |
|
|
 |
|
| |
| |
| |
| |
|
|
 |
Labor
of love
“Being
a midwife is the best job in health care,” says Jane Mashburn,
specialty coordinator for Emory’s Nurse-Midwifery Program
and herself a graduate of its first class in 1978. “Midwifery
lets you work closely with patients, take a holistic view of women’s
health and pregnancy, and view labor as a normal process, not a
medical problem.”
Mashburn is not alone in her thinking.
The program’s core faculty are all practicing midwives, who
have taught and worked together for more than 20 years. According
to Mashburn, they provide a personal learning environment that empowers
students, who have one of the highest pass rates on certification
exams in the country. Another marker of success is the program’s consistent top 10 ranking
in U.S. News & World Report (it currently places seventh).
marker of success is the program’s consistent top 10 ranking
in U.S. News & World Report (it currently places seventh).
The Nurse-Midwifery Program in the
Nell Hodgson Woodruff School of Nursing also draws on partners at
the Centers for Disease Control and Prevention (CDC), the Rollins
School of Public Health, and the Lillian Carter Center for International
Nursing.
For Kitty MacFarlane, who received
both her undergraduate nursing degree and a dual master’s
degree in nursing and public health at Emory, the midwifery program
opened doors to CDC’s Division of Reproductive Health. There,
she works as part of a multidisciplinary team that implements community-based
perinatal surveillance in developing countries. MacFarlane’s
role on the team is to teach midwives how to collect and interpret
surveillance data to improve the use of scarce resources for maternal
and child health program management.
Recently she was awarded funding from
the Gates Foundation to develop a pilot midwife case-management
training program in Afghanistan. The goal of the new initiative
is to introduce safe water systems into the homes of very low birth
weight infants born at a women’s hospital in Kabul. “Training
Afghan midwives for this new, nontraditional role will benefit the
families of these fragile infants, broaden the professional development
of midwives in Afghanistan, and help link the hospital to local
community resources,” says MacFarlane.
Other graduates have chosen to practice
close to where they trained. “Many of our clinical sites are
staffed by alumni,” says Mashburn. “Not many schools
have that.” In addition to working as midwives, the program’s
graduates are involved in careers in health care services research,
nursing education, health care counseling, and community health
education.
This holistic approach to women’s
health reflects the coordinator’s own motivation for entering
the field. “I chose midwifery to be present in a woman’s
life, more than just during her labor,” says Mashburn. “I
wanted to be there for the whole pregnancy.” —Jennifer
Williams |
 |
| |
|
|
 |
| |
|
|
|
|
|
| |
|
|
|
| |
 |
The
RUTH effect
 An
international team of researchers recently completed a clinical
trial to see if the drug raloxifene could affect the heart health
of more than 10,000 women from 26 countries who had experienced
coronary heart disease or were at high risk for a heart attack.
It turns out that raloxifene, marketed as Evista in the United States
for the prevention and treatment of osteoporosis in postmenopausal
women, had no significant effect on coronary events in this trial
group. An
international team of researchers recently completed a clinical
trial to see if the drug raloxifene could affect the heart health
of more than 10,000 women from 26 countries who had experienced
coronary heart disease or were at high risk for a heart attack.
It turns out that raloxifene, marketed as Evista in the United States
for the prevention and treatment of osteoporosis in postmenopausal
women, had no significant effect on coronary events in this trial
group.
However, the study showed positive
impacts in other areas. Raloxifene did reduce the risk of invasive
breast cancer and spinal fractures in the participants, who were
followed for an average of 5.6 years.
Results of the RUTH study (Raloxifene
Use for the Heart) are published in the July 13 issue of the New
England Journal of Medicine. Nanette Wenger, professor of medicine
and chief of cardiology at Grady Memorial Hospital, served as principal
investigator of RUTH at Emory and was the co-principal investigator
for the international study.
“Overall there was no effect
on coronary events—no increase or decrease,” Wenger
says. “The lack of increase is important, given
the adverse coronary events that were seen with estrogen/progestin
therapy.”
The investigators identified several
harmful effects, including an increase in fatal stroke risk and
an increased risk of obstruction of a blood vessel by blood clots.
In deciding whether to prescribe raloxifene, clinicians should weigh
the benefits in reducing the risk of invasive breast cancer and
spinal fractures against the increased risk of blood clots and fatal
stroke, concluded the researchers. |
 |
| |
|
|
 |
|
|
|
| |
|
|
|
| |
TOP
|
|
|
| |
| |
|
|
 |
Three
strikes
Their
cause is unknown, their treatment is difficult, and as of now, their
outcome is questionable. Triple negatives are a newly identified
aggressive form of breast cancer that brings anxiety to women much
too young for such a devastating disease.
Epidemiologist Mary Jo Lund
presented her findings on triple negatives at the recent annual
meeting of the American Association of Cancer Researchers. Preliminary
results of the study indicate that black women may be at higher
risk for worse breast tumors and at an earlier age. Building on
these findings, Lund and a team of researchers from the Rollins
School of Public Health and Winship Cancer Institute are developing a multidisciplinary project to examine triple negative
breast tumors. Key collaborators include Otis Brawley and Ruth O’Regan.
are developing a multidisciplinary project to examine triple negative
breast tumors. Key collaborators include Otis Brawley and Ruth O’Regan.
Triple negatives are characterized
by three biologic components that make this form of breast cancer
difficult to treat. Oncologists base treatment decisions on the
presence of three receptors known to fuel most breast cancers—estrogen
receptors, progesterone receptors, and human epidermal growth factor
receptor 2 (HER2). The most effective agents against breast cancer,
such as tamoxifen and trastuzumab (Herceptin), work by targeting
these receptors. Women with triple negative tumors lack all three.
What is most alarming in the understanding
of this type of breast cancer is its high rate of existence in young
black women. Its chance of occurrence in this population is almost
three-fold more likely than in white women, according to Lund.
Overall, black women are at
lower risk for breast cancer compared with white women. However,
for women under the age of 50, black women are at increased risk
over white women of the same age. And evidence exists that younger
black women have breast tumors with more aggressive features. While
factors such as socio-demographics and systematic disadvantages
may affect the development of these “worst-case scenario”
tumors in black women, the actual cause goes deeper. It reaches
into the genes.
Lund and her colleagues hypothesize
that black women have a genetic disadvantage, which encourages development
of these tumors. The researchers want to learn why this susceptibility
exists. Their multidisciplinary study includes a questionnaire,
blood tests, and collection of tumor samples. It is ongoing at three
Emory-affiliated hospitals in Atlanta among black and white female
patients who live in Fulton and DeKalb counties. These two metro
Atlanta counties account for the majority of breast cancers diagnosed
among black women, particularly those under the age of 50. The researchers
are analyzing tumors and searching for other protein markers, besides
the existing receptors, which occur consistently in triple negatives.
They hope to find other protein markers that occur consistently
enough to open doors for new, protein-targeted treatments. That
approach is good news for women because it will target the tumor
independently, unlike chemotherapy, which “indiscriminately
attacks tumor and normal cells,” Lund says.
Ultimately, the research will give
us a biologic and a non-biologic perspective on this type of breast
cancer, collecting information on genetics, tumor biology, and socio-demographic
factors, she says. “We believe that risk and outcome are inextricably
connected.” —JW
|
 |
| |
|
|
 |
| |
|
|
|
|
|
| |
|
|
|
| |
| |
|
|
 |
We've
come a long way, baby
Used
to be, repair for a broken hip required invasive surgery with a
12- to 18-inch incision, and the replacement of the ball and socket
lasted an average of only 15 years. However, that scenario
has changed dramatically, thanks to recent advances in hip reconstructive
surgery. “With longer-lasting implants and less invasive surgeries,
total hip replacement (THR) now ranks among our most successful
procedures,” says Emory orthopedist Greg Erens.
Emory orthopedic surgeons perform
approximately 600 THRs each year. The American Academy of Orthopedic
Surgeons estimates that more than 193,000 THRs are performed annually
in the United States.
Part of the success orthopedists have
had in extending the life of replacement implants comes from advances
in material science, metallurgy, and manufacturing. Alternative bearing surfaces, such
as the ones Erens uses in his practice, wear less and last longer.
These include cross-linked polyethylene, ceramic-on-ceramic, and
metal-on-metal. By contrast, materials used in previous generations—a
metal ball and polyethylene liner—led to release of small
polyethylene particles as the liner wore out, starting a cascade
of events that could lead to severe bone loss around the hip and
eventually loosening and failure of the implant.
metallurgy, and manufacturing. Alternative bearing surfaces, such
as the ones Erens uses in his practice, wear less and last longer.
These include cross-linked polyethylene, ceramic-on-ceramic, and
metal-on-metal. By contrast, materials used in previous generations—a
metal ball and polyethylene liner—led to release of small
polyethylene particles as the liner wore out, starting a cascade
of events that could lead to severe bone loss around the hip and
eventually loosening and failure of the implant.
Another advantage of today’s
alternative bearings is that patients can be fitted with a larger
head or ball to replace the top of the femur. In the past, larger
head sizes were avoided because they were associated with increased
polyethylene wear, according to Erens. However, the new materials
make it possible to use larger head sizes and thereby increase hip
stability and reduce the risk of a dislocation.
While alternative bearings are more
expensive than standard polyethylene, with ceramic-on-ceramic being
the most costly, the price is minimal when compared to the cost
of a second surgery if the original replacement fails.
Erens and James Roberson, professor
and chair of the Department of Orthopaedics at Emory, are participating
in ongoing studies to track how long this new generation of alternative
bearings will last. Although it is too soon to have final numbers,
their preliminary research is showing positive signs.
In addition to use of innovative materials,
the surgical procedure for THR has undergone dramatic improvements.
THR can now be performed safely and effectively through a minimally
invasive approach with an incision averaging between 3 to 4 inches.
This approach minimizes tissue trauma under the incision and decreases
blood loss. It shortens the surgery time and encourages faster recovery
and rehabilitation. It even eases patients’ anxieties about
the process: a 4-inch incision is less intimidating than an 18-inch
scar.
Erens’s long-term goal is to
deliver the same good news to every THR patient: “Those new
hips will last for a lifetime.” —Stacia M. Brown
|
 |
| |
|
|
 |
| |
|
|
|
|
|
| |
TOP
|
|
|
| |
| |
|
|
 |
First
sight
Emory
ophthalmic surgeon Diane Song is the only physician
in Georgia and one of only a few in the Southeast who perform pediatric
corneal transplants.
While the surgery is one of the most
common transplants among adults, few doctors are comfortable applying
it to children. With a high chance
for tissue rejection and only an average one-in-three chance of success in this age group, they have reason for caution.
chance of success in this age group, they have reason for caution.
Yet a successful surgery and recovery
gives a child the possibility of learning to see rather than remaining
partially blind.
For babies born with vision-impairing
conditions due to opaque cornea such as Peter’s anomaly or
scars from infections, corneal transplants allow for proper development
of vision. Without the transplant, the visual center of the brain
is unable to receive stimuli necessary for development of the capacity
to see. At birth, all babies have poor vision, and as the brain
learns to recognize objects, life comes into focus.
“Time is crucial for this surgery,”
Song says. “The window of opportunity is between three and
four months when the baby is first beginning to respond to visual
stimulation. Most of visual brain development occurs during the
first two years of life. By the time a child reaches school age,
it’s too late.”
However, undergoing the procedure
too early also can be devastating. “The younger the baby,
the higher the chance is for tissue rejection,” says Song.
Unlike other transplants, where organs
are difficult to procure and match, patients needing a new cornea
have just a short wait, and the procedure does not require matching
blood types. After surgery, patients start a regimen of medicated
drops (sometimes lasting for life) to prevent tissue rejection,
infection, and glaucoma—a common association with Peter’s
anomaly.
“Parents and caretakers are
crucial for a successful transplant,” Song says. “If
they are good about applying the drops, taking the child for frequent
follow-up visits, caring for contact lenses or glasses, and recognizing
problems early, then the surgery has a better chance of succeeding.”
Song performs between 10 and 12 pediatric corneal transplants a
year.
The corneal transplant is just the
first step in the process of helping a baby see. Following surgery,
a multi-specialty group of medical professionals is involved in
years of rehabilitation. A specialist fits the baby for contacts,
while a pediatric ophthalmologist treats amblyopia, or lazy eye,
often by patching the good eye and thus training the brain to use
the affected eye. Frequently, a glaucoma specialist is part of the
rehab team.
“A corneal transplant doesn’t
give babies perfect vision,” Song says, “but it does
clear a path for them to develop perfect vision.” —JW
|
 |
| |
|
|
 |
| |
|
|
|
|
|
| |
|
|
|
| |
| |
|
|
 |
 |
Emory
Healthcare was in the right place at the right time at
the 2006 Peachtree Road Race. As the medical provider for the world’s
largest 10K event, the Emory/Grady team successfully saved the lives
of two people who experienced heart attacks at the finish line.
Unfortunately, those stats don’t hold on other days in Atlanta,
which has one of the lowest cardiac arrest survival rates in the
nation, according to Eric Ossmann, medical director of Grady EMS.
What is needed to win the larger daily race? A better coordinated
911 communications system, willing bystanders to start CPR before
paramedics arrive, and more strategically placed defibrillators
in communities and the work place with people trained to use them,
says Ossman. |
 |
| |
|
|
 |
| |
|
|
|
|
|
| |
|
|
|
| |
| |
|
|
|
|
|
|
 |
Milestones
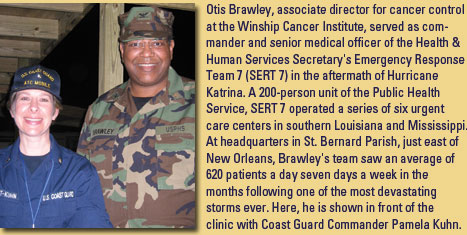
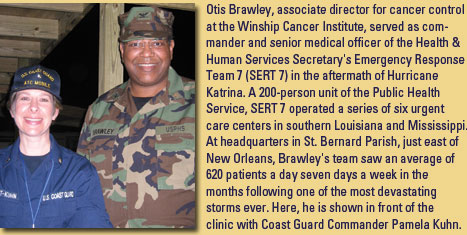
 The
Woodruff Health Sciences Center was among four organizations
honored for its relief efforts to victims of Hurricane Katrina in
the Atlanta Business Chronicle’s annual Healthcare Heroes
awards. Of more than 400 patients who were hospitalized in Atlanta-area
facilities in the early days following the disaster, more than 150
were sent to Emory hospitals. The university played an active role
in ensuring that patients were quickly placed in appropriate hospitals,
and faculty, staff, students, and alumni provided a cadre of volunteers,
staffing shelters for evacuees and providing temporary housing. The
Woodruff Health Sciences Center was among four organizations
honored for its relief efforts to victims of Hurricane Katrina in
the Atlanta Business Chronicle’s annual Healthcare Heroes
awards. Of more than 400 patients who were hospitalized in Atlanta-area
facilities in the early days following the disaster, more than 150
were sent to Emory hospitals. The university played an active role
in ensuring that patients were quickly placed in appropriate hospitals,
and faculty, staff, students, and alumni provided a cadre of volunteers,
staffing shelters for evacuees and providing temporary housing.
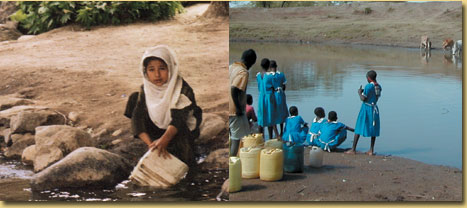
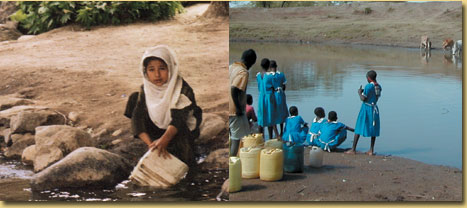
 The
Emory Center for Global Safe Water (CGSW) had two winning
proposals in the World Bank’s Development Marketplace 2006
global competition. A competitive grant program that funds innovative,
small-scale development projects that deliver results and show potential
to be expanded or replicated, the Development Marketplace will support
CGSW projects that use income-generating local enterprises to increase
access to safe water and improved sanitation in poor communities—one
in Bolivia and one in Kenya. Only 30 winners out of more than 2,500
proposals were funded. The
Emory Center for Global Safe Water (CGSW) had two winning
proposals in the World Bank’s Development Marketplace 2006
global competition. A competitive grant program that funds innovative,
small-scale development projects that deliver results and show potential
to be expanded or replicated, the Development Marketplace will support
CGSW projects that use income-generating local enterprises to increase
access to safe water and improved sanitation in poor communities—one
in Bolivia and one in Kenya. Only 30 winners out of more than 2,500
proposals were funded.
 Emory
University was named the top-ranked university and the
No. 4 institution overall in the Best Place to Work for Postdoctoral
Students 2006 survey, conducted by The Scientist magazine. Emory
University was named the top-ranked university and the
No. 4 institution overall in the Best Place to Work for Postdoctoral
Students 2006 survey, conducted by The Scientist magazine.
 Emory University Hospital has been awarded Primary
Stroke Center Certification for its rapid response in diagnosing
and treating stroke patients using a multi-specialty approach and
for efforts to foster better outcomes for stroke care. The hospital
earned the distinction from the Joint Commission of Accreditation
of Healthcare Organizations.
Emory University Hospital has been awarded Primary
Stroke Center Certification for its rapid response in diagnosing
and treating stroke patients using a multi-specialty approach and
for efforts to foster better outcomes for stroke care. The hospital
earned the distinction from the Joint Commission of Accreditation
of Healthcare Organizations.
 Solucient, the nation’s leading source of
healthcare information products, has named EUH as one of 100 hospitals
making the greatest progress in improving hospital-wide performance
over five years. The hospital is setting a national benchmark for
consistent improvement in clinical outcomes, safety, hospital efficiency,
financial stability, and growth.
Solucient, the nation’s leading source of
healthcare information products, has named EUH as one of 100 hospitals
making the greatest progress in improving hospital-wide performance
over five years. The hospital is setting a national benchmark for
consistent improvement in clinical outcomes, safety, hospital efficiency,
financial stability, and growth.
 The Emory Clinic’s Department of Radiation Oncology
received the 2006 Outpatient Excellence Award for Oncology Centers
from Outpatient Care Technology magazine.
The Emory Clinic’s Department of Radiation Oncology
received the 2006 Outpatient Excellence Award for Oncology Centers
from Outpatient Care Technology magazine.
 The Carter Center has received a 2006 Gates Award
for Global Health from the Bill & Melinda Gates Foundation in
recognition of its work to fight neglected diseases such as Guinea
worm, river blindness, and lymphatic filariasis. The $1 million
award, the world’s largest prize for international health,
honors extraordinary efforts to improve health in developing countries.
The Carter Center has received a 2006 Gates Award
for Global Health from the Bill & Melinda Gates Foundation in
recognition of its work to fight neglected diseases such as Guinea
worm, river blindness, and lymphatic filariasis. The $1 million
award, the world’s largest prize for international health,
honors extraordinary efforts to improve health in developing countries.
|
 |
| |
|
|
 |
|
|
|
| |
|
|
|
| |
|
|
|
| |
|
|
|




 emergency room. Another IOM committee on which Kellermann served
calculated that U.S. hospitals and doctors lose billions annually
in uncompensated care of the uninsured, which in turn creates enormous
stress on the health care system. In the 2004 fiscal year, uncompensated
care provided by Emory physicians at Grady totaled $22 million.
(Emory Healthcare provided $51.7 million that year
emergency room. Another IOM committee on which Kellermann served
calculated that U.S. hospitals and doctors lose billions annually
in uncompensated care of the uninsured, which in turn creates enormous
stress on the health care system. In the 2004 fiscal year, uncompensated
care provided by Emory physicians at Grady totaled $22 million.
(Emory Healthcare provided $51.7 million that year The
idea is no small one: to relocate Emory University Hospital to the
east side of Clifton Road alongside a new clinic cluster for outpatient
care, medical faculty offices, and medical research. But
the Emory Board of Trustees is thinking large-scale and long-term,
and in June, it officially accepted the results of a nine-month
feasibility study. Following the recommendation of the Woodruff
Health Sciences Center board, the University’s Board of Trustees
authorized preparation of architectural schematic designs for new
hospital and outpatient facilities that could take as long as a
decade and as much as $2.2 billion to realize.
The
idea is no small one: to relocate Emory University Hospital to the
east side of Clifton Road alongside a new clinic cluster for outpatient
care, medical faculty offices, and medical research. But
the Emory Board of Trustees is thinking large-scale and long-term,
and in June, it officially accepted the results of a nine-month
feasibility study. Following the recommendation of the Woodruff
Health Sciences Center board, the University’s Board of Trustees
authorized preparation of architectural schematic designs for new
hospital and outpatient facilities that could take as long as a
decade and as much as $2.2 billion to realize.
 Support
for creating specialized health courts is growing. U.S.
Senate Majority Leader Bill Frist and the Progress Policy Institute,
known in the 1990s as President Clinton’s “idea mill,”
have endorsed the concept. So have more than 80 leaders in U.S.
health care, including Woodruff Health Sciences Center CEO Michael
Johns, and a broad coalition of patient advocates and health care
providers, including Emory Healthcare. Known as Common Good, the
bipartisan legal reform group is championing such courts as a way
to restore reliability to medical justice.
Support
for creating specialized health courts is growing. U.S.
Senate Majority Leader Bill Frist and the Progress Policy Institute,
known in the 1990s as President Clinton’s “idea mill,”
have endorsed the concept. So have more than 80 leaders in U.S.
health care, including Woodruff Health Sciences Center CEO Michael
Johns, and a broad coalition of patient advocates and health care
providers, including Emory Healthcare. Known as Common Good, the
bipartisan legal reform group is championing such courts as a way
to restore reliability to medical justice. combining with other substances) and pro-oxidants in cells. The
damage included structural changes as the protein accumulated additional
oxygen molecules.
combining with other substances) and pro-oxidants in cells. The
damage included structural changes as the protein accumulated additional
oxygen molecules.  than 80, computer and Internet access for patients, education
classrooms, evaluation suites with multi-media capability, 20 exam
rooms, increased infusion room capacity, advanced biopsy procedure
rooms with high-tech ultrasound equipment, and expanded clinical
lab space.
than 80, computer and Internet access for patients, education
classrooms, evaluation suites with multi-media capability, 20 exam
rooms, increased infusion room capacity, advanced biopsy procedure
rooms with high-tech ultrasound equipment, and expanded clinical
lab space. marker of success is the program’s consistent top 10 ranking
in U.S. News & World Report (it currently places seventh).
marker of success is the program’s consistent top 10 ranking
in U.S. News & World Report (it currently places seventh). An
international team of researchers recently completed a clinical
trial to see if the drug raloxifene could affect the heart health
of more than 10,000 women from 26 countries who had experienced
coronary heart disease or were at high risk for a heart attack.
It turns out that raloxifene, marketed as Evista in the United States
for the prevention and treatment of osteoporosis in postmenopausal
women, had no significant effect on coronary events in this trial
group.
An
international team of researchers recently completed a clinical
trial to see if the drug raloxifene could affect the heart health
of more than 10,000 women from 26 countries who had experienced
coronary heart disease or were at high risk for a heart attack.
It turns out that raloxifene, marketed as Evista in the United States
for the prevention and treatment of osteoporosis in postmenopausal
women, had no significant effect on coronary events in this trial
group.  are developing a multidisciplinary project to examine triple negative
breast tumors. Key collaborators include Otis Brawley and Ruth O’Regan.
are developing a multidisciplinary project to examine triple negative
breast tumors. Key collaborators include Otis Brawley and Ruth O’Regan.
 metallurgy, and manufacturing. Alternative bearing surfaces, such
as the ones Erens uses in his practice, wear less and last longer.
These include cross-linked polyethylene, ceramic-on-ceramic, and
metal-on-metal. By contrast, materials used in previous generations—a
metal ball and polyethylene liner—led to release of small
polyethylene particles as the liner wore out, starting a cascade
of events that could lead to severe bone loss around the hip and
eventually loosening and failure of the implant.
metallurgy, and manufacturing. Alternative bearing surfaces, such
as the ones Erens uses in his practice, wear less and last longer.
These include cross-linked polyethylene, ceramic-on-ceramic, and
metal-on-metal. By contrast, materials used in previous generations—a
metal ball and polyethylene liner—led to release of small
polyethylene particles as the liner wore out, starting a cascade
of events that could lead to severe bone loss around the hip and
eventually loosening and failure of the implant. chance of success in this age group, they have reason for caution.
chance of success in this age group, they have reason for caution.