|




|
| |
|
|
 |
| |
|
|
 |
Mr.
G, a 45-year-old Mexican immigrant undergoes an employment health
screening and learns he has dangerously high blood pressure. He
is told he will not be permitted to work until his condition is
under control. He goes to a local Georgia emergency room for treatment
and is given a beta-blocker and diuretic, each to be taken once
a day.
One week later, the man presents in
the same emergency room complaining of dizziness. An examination
shows he now has dangerously low blood pressure. He tells the nurse
he has been taking his medicine just as it says to on the labels.
This confuses the care team until a physician fluent in Spanish
asks him how many pills he takes each day. His reply is “22.”
The doctor then explains to his colleagues
that the word “once” (pronounced “ohn SAY”)
is Spanish for 11. Fortunately, the patient’s condition is
stabilized, and he suffers no serious harm. |
 |
| |
|
|
 |
Six
years ago, this near miss would likely have been just another anecdote
or “learning experience” shared by a few colleagues.
But the day after this incident, a hospital administrator sends
a report to the Georgia Hospital Association’s Partnership
for Health Accountability (PHA) describing what happened and asking
for help in preventing similar incidents.
Although this case is hypothetical,
it’s typical of problems routinely reported to the PHA through
its five-year-old voluntary medical-error reporting system.
Such candor would have been unthinkable
when the system first started, says Vi Naylor, executive vice president
of the hospital association, which launched the partnership in 2000.
“Hospitals were very concerned about confidentiality and reluctant
to share information.”
Envisioning the banner headlines and
civil lawsuits that are so often the result when medical mistakes
are made public, administrators blanched at the thought of voluntarily
sending out sensitive data statewide.
“But over time we developed
their trust,” Naylor continues. “They have seen that
we are able to share information and still maintain the security
of what they send us.” Participating hospitals fill out sentinel-event
forms and receive fast, confidential feedback from other hospitals
on issues requiring urgent attention. They also regularly report
aggregate data on medication errors, incidence of pressure ulcers,
and other common problems to a centralized database. Hospitals can
choose to report information in all categories or just select individual
areas to focus on. The association analyzes this information and
prepares a report comparing each hospital with other institutions
of similar size and capability across the state. Periodic teleconferences
also provide a forum for sharing experiences and strategies.
Today, administrators from across
the state frequently call to suggest ideas for safety alerts and
share concerns and problems they have had, Naylor says. |
 |
| |
|
|
 |
| |
|
|
 |
A
national model?
Georgia’s
system has the potential to become a model for other states, says
Ken Thorpe, director of the Emory Center for Health Outcomes and
Quality (CHOQ) at the Rollins School of Public Health, which is
working with the GHA to evaluate and improve the system’s
effectiveness.
Formed in 2001, the CHOQ is one of
the largest research centers in the nation devoted exclusively to
evaluating and measuring the quality of health care. Research teams
partner with other groups, such as health care providers, large
group purchasers of health services, and private insurers, to evaluate
problems and design interventions.
“Georgia has, to my knowledge,
the first statewide voluntary reporting system in the country,”
says Thorpe. “If you can make a system like this work—if
it helps reduce medical errors and encourages providers to focus
on areas they want to improve—it can have important national
implications.”
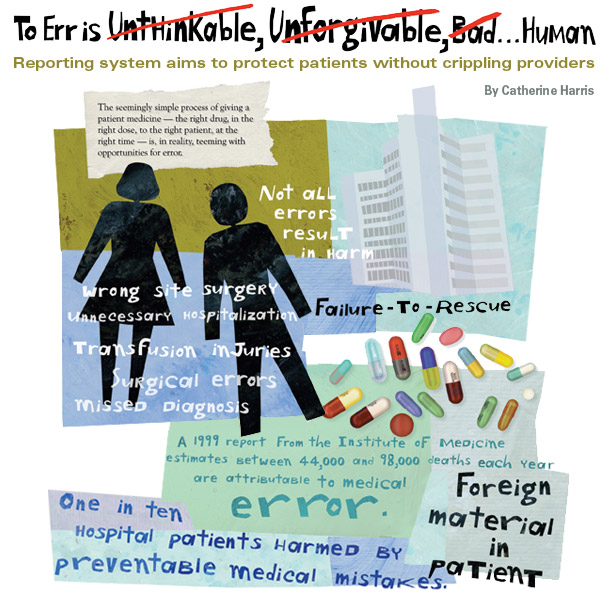
Hospitals across the country have
been under fire since a 1999 report from the Institute of Medicine
estimated the number of people killed by medical errors in hospitals
each year to be between 44,000 and 98,000. The report sparked a
nationwide push for more oversight of health care providers, particularly
hospitals. Several states passed laws establishing mandatory reporting
systems, which publicly rank hospitals by the quality of care they
provide as determined by the number of errors reported.
But many providers believe these efforts
are flawed. Systems designed to measure quality often evaluate small
community hospitals by the same benchmarks used for large, urban
academic medical centers, with the result that neither is evaluated
fairly. Large centers have more resources but also see much sicker
patients and therefore have higher rates of death and other poor
outcomes. Many initiatives also base their rankings on information
obtained from data sets not designed to measure quality of care.
Even the term “medical error”
can be confusing. Clearly, prescribing the wrong medicine or amputating
the wrong limb counts. But what about the patient with limited literacy
skills who takes 10 times the appropriate amount of medication because
he can’t read the bottle’s label? Or a surgical patient
with multiple co-existing medical conditions who gets an infection
while in the hospital? Should poor outcomes that are the result
of many complicated factors be reported as medical mistakes?
At the same time, rising rates for
malpractice coverage give hospitals powerful incentive to hide,
not report, any problems they have with patient safety. In some
states, information about hospital quality-improvement projects
can still be “discoverable” by attorneys in a malpractice
case, who then use the institution’s effort at correcting
a problem as evidence that the institution was at fault.
“In the states that have mandatory
reporting, one of the key concerns is that you don’t actually
get much reporting,” says Thorpe. “Because of liability
concerns, hospitals are reluctant to report information to the databases.
So the institutions that end up with higher rates of mortality,
medication errors, or whatever is being measured are often the ones
who have been most proactive about reporting—they are the
ones paying attention to this. Other hospitals may report lower
rates simply because they are not as vigilant about looking for
mistakes or problems. Some systems actually penalize the behavior
you want to encourage.” |
 |
| |
|
|
 |
| |
|
|
 |
How
hospitals miss the mark
Georgia’s
system—with its emphasis on communication, correcting problems,
and finding best practices—has been key to encouraging hospitals
to move closer toward the “culture of safety” necessary
to truly improve, says Bill Bornstein, chief quality officer for
Emory Healthcare, which participates in the reporting system and
has won three of its statewide quality awards.
“In health care, errors are
grossly under-reported,” he states. “And this is not
entirely due to liability issues. The punitive culture also contributes.
Using error-rate reporting comparatively in and of itself incentivizes
against reporting.”
For too long, he says, the nation’s
health care industry has adhered to the belief that mistakes are
the result of individual error and that if all people hired to work
in a health care facility are willing to work hard, are trained
appropriately, and are always diligent, then mistakes won’t
happen.
However, other industries also charged
with maintaining the safety of large numbers of people—notably
the aviation industry—have rejected this kind of thinking.
Aviation now follows total quality
management and quality-improvement processes that focus on identifying
potential problems before they escalate to the point that an accident
can occur. The goal is designing systems and practices to eliminate
the potential for mistakes to occur.
“They accept the concept that
human error is inevitable and predictable in terms of frequency,
and that if you want to avoid errors resulting in harm, you must
design systems to intercept and prevent the occurrences before they
lead to harm,” Bornstein says.
Implementing a culture of safety means
that health care facilities must look at incidents as evidence of
a system failure in need of correction instead of wasting effort
trying to decide whether a bad outcome was the result of a “mistake,”
he says.
A good example of this shift in philosophy
is Emory Hospital’s correct-site surgery protocol, now the
model used by the PHA to develop its statewide guidance for other
hospitals. Emory’s protocol was developed in the late 1990s,
well before the 2003 Joint Commission on Accreditation of Healthcare
Organization’s decision requiring hospitals to implement similar
processes, he says.
The policy is continually reevaluated
and has since been expanded to include all invasive procedures performed
at Emory Hospitals and The Emory Clinic.
“We use a three-pronged approach
ensuring we have ascertained the following for each procedure: (1)
the correct patient, (2) the correct procedure, and (3) the correct
site,” says Jane Vosloh, director of nursing, perioperative
and endoscopic services for Emory Hospitals.
When a patient is admitted to the
unit, providers must verify the person’s identity and ensure
that critical information—particularly a current history and
physical examination and documentation of informed consent—are
included in the chart. Once that process is complete, the patient
is given a colored armband identifying the service to which he or
she is admitted.
The correct site of surgery is also
clearly marked on the patient. And the policy prohibits caregivers
from marking up the surgery site (or proceeding with planning for
the procedure) without reverifying the patient’s identity
and the planned procedure against the information in the chart,
documenting both verifications in the record.
Several checks and balances are built
into the protocol, so that even if one person forgets to perform
a check, someone else down the line has the same responsibility,
says Vosloh.
Finally, prior to the start of the
procedure, a mandatory time-out (officially known as the “call
to order”) is taken for a final check of the patient’s
identity, site of surgery, and the procedure to be performed.
At first, many surgeons resisted taking
all of the steps required, says Vosloh. They considered it a point
of professional integrity to “know their patient” without
repeatedly checking his or her identification.
However, one memorable incident several
years ago convinced many.
“We had a near miss,”
she says. “We got down to the call to order and did the check
and realized we had prepped and draped the wrong side of the patient.”
The error was caught in time and corrected,
but it demonstrated how mistakes happen to even the best providers.
“It also proved that the policy
worked as it was designed to—we caught the mistake and prevented
surgery on the wrong site,” she says. “It made a lot
of people realize we really did need a protocol.” |
 |
| |
|
|
 |
| |
|
|
 |
Initial
success
Emory’s
CHOQ research indicates that the Georgia system is both improving
the quality of patient care and attracting hospital participation.
Analysis of the data collected over the past five years shows a
35% mean decrease in reported error rates overall, says Kim Rask,
a practicing physician and center researcher who holds joint appointments
in both public health and medicine.
All of Georgia’s hospitals participate
in at least one of the PHA’s reporting initiatives, she notes.
The medication-error initiative is the most popular, and most hospitals
participate in at least two. A recent evaluation of medication-error
data found that 80% of participating hospitals have lowered their
error rates.
“Even for the 20% that saw no
improvement or saw their rates get worse, we are encouraged that
they were willing to report those findings and that they continued
to participate and try to improve,” says Rask. “If everyone
had done better, you would always have to wonder about your reporting.
“So it does seem that people
are putting interventions in place, the vast majority are improving,
and the others have the opportunity to learn from their peers.”
|
 |
| |
|
|
| |
|
|
| |
|
|
|
|
| |
 |
Building
a Better Report Card |
 |
|
| |
|
|
|
|
 |
 |
When
the Institute of Medicine’s report, To Err is Human,
was released, officials at the Georgia Hospital Association
(GHA) knew they had to act quickly, says association president
Vi Naylor.
“We had a limited window
to develop a reporting system that we felt would be accurate
and would help improve patient safety—or have one imposed
on us from the outside,” she says.
The GHA’s first step was
establishing the Partnership for Health Accountability (PHA)
and getting its Accountability and Health Safety Committee
recognized as a state peer-review organization. Georgia’s
state peer-review law protects information collected for the
purpose of improving patient care from public disclosure and
legal discoverability. The PHA then set up a reporting system
to track medication errors and a select number of other medical
events.
The reporting system is completely
voluntary—hospitals are not punished for not submitting
data, but if they choose to do so, they gain access to information
about how their data compare with those of other hospitals
of comparable size and type, as well as information about
evidence-based best practices. The PHA also sponsors periodic
telephone conferences that allow administrators at different
facilities to share ideas and experiences.
And although the reporting system
is nonpunitive, the PHA does require hospitals that report
medical errors or near misses to submit a plan of correction
and then periodically submit reports detailing its implementation,
says Naylor. “If they do not, they can no longer participate
in the program. So far, we have not had that happen.”
The system provides confidentiality
for reporting of medical errors and sentinel events, but the
GHA also believes public accountability is vital. Each year,
the PHA publishes a report, “Insights,” (available
on their website at www.gha.org/pha) which lists each hospital
by county and indicates whether it participates in both national
and statewide quality-improvement initiatives. A separate
section details whether each hospital meets certain care benchmarks
set by the Joint Commission on Accreditation of Healthcare
Organizations and the Centers for Medicare and Medicaid Services.
|
 |
 |
| |
|
|
|
|
|
| |
|
|
| |
Catherine
Harris is the editor of Momentum. |
|
| |
|
|
| |
|
|
|
|
|

