By Quinn Eastman • Illustration by Bryan Christie
In April 1947, two doctors at Emory University Hospital saw something they had never seen before.
Their patient was a 55-year-old man who complained of chest pain, had difficulty breathing, and had lost 30 pounds in the previous three weeks. A routine chest X-ray showed nothing helpful to Heinz Weens, Emory’s first chair of radiology, and his colleague Abner Golden.
The two radiologists decided to perform an angiocardiogram—at the time, a relatively new procedure. By injecting dye into the man’s heart, they could see the spaces in his arteries where blood flows. From what they saw, they guessed the patient had a dissecting aneurysm, a serious condition in which the inner layer of his aorta had torn away.
Previously, no one had ever known what a dissecting aneurysm looked like on an angiocardiogram, as they later reported in the American Heart Journal.
Their diagnosis proved correct. Surgeons opened the patient’s chest and repaired his aorta with cellophane. Six months later, he had gained 10 pounds.
Fast forward almost 60 years to another hard-to-diagnose patient at Emory. After being injured in a car crash, a 45-year-old woman began stuttering, had difficulty naming objects, and experienced tremors in her right hand and foot. Using standard imaging techniques, her doctors were unable to detect any brain damage.The patient was suspected of faking the symptoms and was denied disability benefits.
However, when she came to Emory, radiologist Hui Mao and his colleagues took a closer look with new technologies, and they did find something. Mao’s team used a combination of functional magnetic resonance imaging (fMRI), which maps brain activities while a person performs a specific task, and diffusion tensor imaging (DTI) to diagnose the problem. By measuring restrictions on the ability of water molecules to move in different directions, DTI outlines the paths of axons in the brain, the transmission lines for the electrical signals sent
by nerve cells.
Mao’s group found that the woman had weakened brain activation during speech and fewer-than-normal intact axons connecting two lobes of the left hemisphere of her brain. The Emory scientists think that damage to the parts of the patient’s brain responsible for grammar and word generation led to her stuttering and difficulty in forming a sentence, as they reported in the Journal of Neuroimaging.
Although DTI is still experimental and most hospitals lack the equipment and expertise to use it, Mao’s team has validated it as a diagnostic tool for brain injuries. Now they are working to further develop this tool to study brain changes associated with aging and neurodegenerative disease and to research the effect of radiation and chemotherapy in patients with brain tumors.
| ny | tiny font | ny |
"The profusion of new technologies challenges radiologists, engineers, and medical educators, because understanding these tools requires expertise and collaboration from so many disciplines." |
||
—Emory Radiologist Hui Mao |
As these cases illustrate, imaging technology has grown increasingly complex in the past 60 years. Doctors have more choices of tools for looking inside the body without cutting it open: not only X-rays but also magnetic fields, radioactive chemicals, and ultrasound.
“The profusion of new techniques challenges radiologists, engineers, and medical educators,” Mao says, “because understanding these tools requires expertise and collaboration from so many disciplines.”
Accompanying this increased complexity is a growing demand for advanced imaging procedures, contributing to rising health care costs. At the same time, the information explosion sometimes brings confusion for patients and doctors alike. The annual number of computed tomography (CT) scans in the United States has roughly doubled in the past decade, raising concern about X-ray exposure.
Researchers at Emory are rising to the challenge by developing smarter imaging. They are improving existing technology to obtain more information, adding stereo capabilities to mammography, for example, to reduce false positives without increasing costs. They are combining imaging tools like MRI, DTI, and others to enhance diagnosis and treatment. They are developing better radioactive probes for use in finding prostate and brain tumors and the amyloid plaques that characterize Alzheimer’s. And increasingly, they are moving past anatomy to visualize function, as the tools of molecular biology filter into the clinic.
Imagine seeing a recovering drug addict’s attendance at a 12-step meeting—from the brain’s point of view. Psychiatry researcher Clint Kilts can do that.
“For the past few years, to use a car analogy, we’ve been concentrating on the accelerator to define the phenomenon of craving in the brain,” he says. “Now, we’re focusing on the brakes. If the brakes are faulty, we want to know how to get them working again.” By brakes, Kilts means processes within the brain that help reformed addicts resist the urge to yield to intense cravings. He has teamed up with addiction specialists at the Atlanta Veterans Affairs Medical Center (VAMC) to study a group of cocaine-dependent men enrolled in a treatment program for substance abuse.
In the study, the researchers ask the men to perform a repetitive task such as counting words displayed on a screen. Occasionally, words are displayed to distract them and evoke memories of their crack-hunting days, words like “payday” or “brillo” (part of a homemade pipe). The researchers simultaneously scan the participants’ brains with fMRI methods that measure blood flow, and those distractions show up on the resulting image.
Such imaging shows clear changes in those who have successfully completed treatment. The scans allow Kilts to visualize increased activity in part of the brain called the ventral medial prefrontal cortex. He postulates that the key to treatment is enhancing a process called extinction, during which the brain forms new neuronal connections that inhibit old habits. The activation that Kilts visualized in the prefrontal cortex reflects a process going on throughout the brain’s circuitry, he says. Such circuits are potential targets for an experimental drug, D-cycloserine, which is thought to enhance extinction and is currently part of an ongoing clinical trial at the VAMC.
| y | y | y | y | y |
| Hui Mao has validated an experimental technology, diffusion tensor imaging, as a diagnostic tool for brain injuries. |
Building on MRI, John Oshinski is developing a computer program to better diagnose what is informally known as sloshing of the heart. |
Carolyn Meltzer is using imaging to study the amyloid plaques that build up in the brain and are associated with Alzheimer’s. |
“For prostate cancer, there’s no equivalent to the mammogram, which is relatively inexpensive and routine,” says Mark Goodman, director of Emory’s radiopharmaceutical discovery lab. Urologists and oncologists agree that current methods for diagnosing prostate cancer—physical exams and the blood test for prostate-specific antigen—are inadequate. Compounding the problem, many prostate tumors grow slowly and take years to turn deadly. Treatment can leave men impotent, incontinent, or both, raising questions as to whether an aggressive approach after first detection is necessary.
In the past, clinicians have tried to use positron-emission tomography (PET) to visualize prostate tumors. The technique involves injecting a radioactive chemical into the body and imaging its distribution. But the most widely used chemical, radioactive glucose, has a specific drawback in the prostate. Glucose, a rapidly excreted sugar, collects in the bladder within minutes and overshadows the area of interest.
Emory radiologists have teamed up to test new ways to map prostate tumors and determine how deadly they could be. Goodman has developed an amino acid probe that prostate tumor cells take up readily. Radiologist David Schuster is leading a clinical trial to test the probe’s potential for diagnosis. And Goodman is leading a separate trial to test the probe as a way to look at brain tumors—hard to see using radioactive glucose because the brain consumes glucose so voraciously.
| ny | tiny font | ny |
"Combining MRI and PET allows you to overlay functional information on top of anatomical information." |
||
—John Votaw, Emory's Director of PET physics and computing |
German engineering giant Siemens is building one of the world’s three combined MRI/PET prototypes for Emory. Siemens is developing the hardware, while Emory scientists are developing the software and applications. “Combining MRI and PET allows you to overlay functional information on top of anatomical information,” says John Votaw, Emory’s director of PET physics and computing.
One advantage of combining MRI’s spatial resolution and PET’s physiologic probing will be less blurring, Votaw says. A PET scan takes about 10 minutes, and if the subject moves, the quality of the image suffers. A person undergoing a PET brain scan wears a device connected to a camera that corrects for head motion. With combined MRI/PET, MRI data replaces the camera.
In addition, combined MRI/PET allows doctors to aim their anti-tumor weapons more accurately. It also allows them to see the effects of radiation and chemotherapy on tumors more quickly.
PET probes can identify dying cells, while MRI can look for growth of aberrant blood vessels in the treated tumor. “The current standard of care is that patient and physician have to wait four to six weeks to see if a tumor changes in size,” Votaw says. “We’re aiming to evaluate a treatment after a week.”
| ny | tiny font | ny |
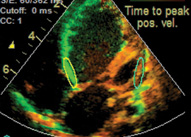
| Cardiac dyssynchrony: when the two sides of the heart beat separately |
Cardiac MRI specialist John Oshinski remembers when his father had a heart attack in 1968. “His doctors couldn’t really do much for him,” he says.
Treatment options for heart ailments have come a long way since then, and imaging continues to play a major role in ensuring such progress. Oshinski and colleagues, for example, are developing methods to more accurately diagnose a condition called cardiac dyssynchrony, in which the two sides of the heart beat separately. The condition affects about one-third of the estimated 5 million people with chronic heart failure in the United States.
“Informally, cardiologists call it ‘sloshing,’” Oshinski says. “The heart spends half its energy just pushing its own walls around rather than pushing blood out to the body.”
In the past five years, doctors have begun using biventricular pacemakers to treat dyssynchrony, with remarkable success in prolonging life. The pacemaker forces all the parts of the heart to beat together. Even so, pacemakers fail to help one-third of those diagnosed with dyssynchrony, in some cases, Oshinski says, because the electrical leads of the pacemakers are inserted into muscle that already has turned to scar tissue.
MRI can help doctors refine their diagnosis and help pinpoint areas for placement of leads. Doctors currently judge patients to have cardiac dyssynchrony using a two-dimensional gauge. If the two halves of the heart’s electrical signals separate enough so that together, their combined peak on an electrocardiogram spans more than 120 milliseconds, it’s considered dyssynchrony.
Using 3D images obtained with MRI, Oshinski’s group is developing computer programs that compare the speed of each heart wall’s movement and calculate changes in volume on each side. In the 40 patients they have evaluated so far, their method, compared with standard electrocardiography, appears to diagnose dyssynchrony with greater precision.
Their programs analyze images already gathered on heart failure patients in many hospitals. “Using this tool is a relatively inexpensive addition,” Oshinski says. “All you need is software.”
If Heinz Weens could see the advances in imaging technology, he’d no doubt be amazed at the ability to visualize subtle problems, such as addiction and neurodegenerative disease. In fact, he’d probably want to know more—for example, how imaging can more directly benefit patients and guide new clinical interventions.
In 1947, the surgery to repair the patient’s heart came directly after Weens took a picture of it. Today, surgeons use real-time MRI scans to guide their instruments during surgery. Researchers hope the future will bring even better ways to plan and see the effects of therapies, whether surgical or noninvasive.
Emory experts say that diagnostic imaging and treatment will continue to be increasingly interwoven. Their prediction is borne out in current studies of the amyloid plaques that build up in the brain and are a hallmark of Alzheimer’s disease. Radiology chair Carolyn Meltzer says that patients with plaques need to be followed closely before they show signs of Alzheimer’s. This is because the role of plaques in Alzheimer’s development is still a subject of debate and question. “Many people accumulate amyloid for years without showing cognitive impairment,” Meltzer says.
Researchers are just now designing treatments that target amyloid. “The most interesting challenge will be to couple sophisticated imaging with these targeted strategies,” says Meltzer.
Will radio advertisements one day offer amyloid PET scans, just as they do now for cardiac CT? It seems plausible. But one thing’s for sure—it’s a ways off. “We need more longitudinal studies of patients as they develop Alzheimer’s to know what we’re looking at,” Meltzer says. “We may need a decade of experience to understand this technique fully."
Seeing smarter is bound to be part of the journey.
Quinn Eastman is a science writer for Emory Health Sciences Communications.
Current Issue | Past Issues | Contact Us | Make a Gift
Back to Top | WHSC home
© 2008. Emory University, All rights reserved.
Back to Top | WHSC home
© 2008. Emory University, All rights reserved.