







 |
 |
| |
|
|
| |
 E-mail
to a Friend
E-mail
to a Friend
 Printer Friendly
Printer Friendly |
|
| |
|
|
| |
Worldwide,
the nursing shortage is increasing at an alarming rate.
In Zambia, 27 of every 1,000 health care workers die of HIV/AIDS.
In the United States, without intervention, the nursing shortage
will reach 1 million by 2012. In Uganda, there are on average only
one or two nurses for every 100 patients. Canada's nursing
shortage is expected to reach 113,000 by 2008.
Certainly migration of health care
workers from poor to wealthier countries that offer better pay and
working conditions contributes to the shortage in many developing
countries. But what causes shortages in wealthier nations? The reasons
are not totally clear-cut, and neither are possible solutions to the global shortage, according to participants
of the 2006 Global Government Health Partners Forum held in November.
possible solutions to the global shortage, according to participants
of the 2006 Global Government Health Partners Forum held in November.
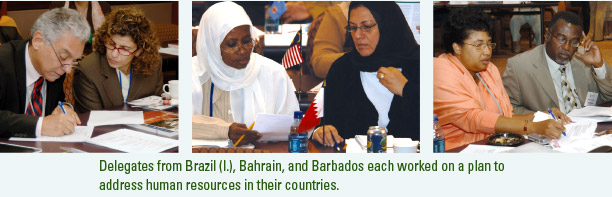
The
conference, hosted by the nursing school's Lillian Carter
Center for International Nursing (LCCIN) and secretariat for the
biennial conference, brought together chief nursing officers (CNOs)
and chief medical officers (CMOs) from 107 countries to address
national and international nursing workforce issues. During the
forum, participants examined workforce roles and responsibilities
and models of collaboration based on current scientific findings,
shared lessons learned, and developed partnership strategies to
enhance their response to public health crises. The CNO/CMO dyads
from each country collaborated to develop a statement of priorities
and a plan of action to address challenges in their own countries.
The
conference built on the successes of the 2001 and 2004 meetings
involving CNOs who developed their leadership skills and built bridges
with one another to address common nursing issues. The landmark
2001 conference marked the first time many CNOs met their regional
counterparts and heard from nursing association and government leaders,
while the 2004 forum was the first of its kind to bring together
CNOs and CMOs in a collaborative, partnership-building effort.
"The
value of the forum extends beyond health leaders detailing the myriad
forces challenging today's health systems," says Dr.
Marla Salmon, secretariat co-chair, dean of the nursing school,and
LCCIN director. "It helped these senior government health
leaders formulate plans to address the challenges and at the same
time create manageable action plans to positively influence the
push-pull factors, such as work conditions, in their own countries
and regions." |
|
| |
|
|
 |
| |
|
|
| |
Examining
workforce migration
Workforce
migration begins within countries as health care workers move from
rural to urban areas and then from the public to the private health
sector. Then the pattern shifts from developing countries to industrialized
ones. The effects of such migration on many regions are both profound
and frustrating. Africa, for example, carries 25% of the world's
burden of disease but has only 1.3% of the world's health workers. In Nigeria, 18% of the country's doctors are abroad,
and there are more Malawian doctors in Manchester, England, than
in Malawi itself. After Africa, South America and the Middle East
face the next highest shortage of health care workers, particularly
nurses.
workers. In Nigeria, 18% of the country's doctors are abroad,
and there are more Malawian doctors in Manchester, England, than
in Malawi itself. After Africa, South America and the Middle East
face the next highest shortage of health care workers, particularly
nurses.
"The full magnitude and impact
of the global shortage of health workers is more evident than ever
before," says Dean Salmon. "The crisis cuts across all
sectors of health care with critical shortages of nurses, as well
as doctors. Collaboration within and across the sectors is imperative
in today's world."
Many countries are seeking ways to retain nurses in regions like
these, where the nurses who remain behind are the ones who bear
the brunt of the day-to-day hardships brought on by such shortages.
Dr.
Manuel Dayrit of the World Health Organization (WHO) told attendees
that in countries where the education of nurses is subsidized by
government funds, the government loses its investment when these
nurses migrate. "Use of tax income to fund nurses' training
does not provide a good return on investment in countries whose
graduates migrate to another country because when they leave the
government loses its investment," he said. The Philippines,
by contrast, which has a large private sector to provide nursing
education, produces thousands of nurses, many of whom migrate. In
this instance, while there may be no direct loss of government investment,
the loss of health professionals from migration affects the health
system in other ways.
Other
developing countries, like Malawi, are using foreign aid (from Great
Britain in this case) to raise the salaries of health care workers.
But countries don't always have discretion in spending these
kinds of resources. Dr. Wilmer Beteta Lopez, Nicaragua's CMO,
said the international loan agreement he works under does not allow
him to adjust salary levels for nurses in more expensive regions
of his country, making retention especially difficult in those areas.
While
salary is extremely important, it is not the only issue that drives
nurses even in the poorest countries to migrate or to leave the
health workforce entirely, according to one presenter's research.
Barbara Stillwell is a senior technical adviser with Liverpool Associates
in Tropical Health and runs a project funded by the U.S. Agency
for International Development to build capacity of the health care
workforce worldwide. She studied nurses in Uganda and found fewer
than half of those interviewed said they were satisfied with their
jobs. While satisfaction with their salary was the most common complaint,
nurses also wanted
to feel valued.
"People
find motivation through their workplace relationships," she
said. "Providing motivation is not necessarily expensive,
but you must have management in place to do that. Feeling valued
will influence productivity, performance, and also retention."
Her study found nurses stayed on the job when their workload was
more manageable, when they actively participated in creating a better
health care facility, and when they were recognized for good work.
|
|
| |
|
|
| |
| |
|
|
 |
Celebrating
Leaders in Health |
 |
| |
|
|
 |
 There's
a conspiracy among chief nursing officers (CNOs), Dr. Jean
Yan says. There's
a conspiracy among chief nursing officers (CNOs), Dr. Jean
Yan says.
"The CNOs conspire to
make sure you succeed," she said after receiving a 2006
Global Health Leadership Award from the Lillian Carter Center
for International Nursing.
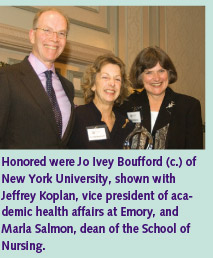
Yan, along with Dr. Jo Ivey
Boufford and Dr. David Nabarro, were recipients of the awards,
handed out at the Global Government Health Partners Forum
2006 in November. The awards are a "celebration of the
partnership of leadership and hope," said Dr. Marla
Salmon, dean of the Nell Hodgson Woodruff School of Nursing.
Yan has been a nurse for 35
years and now is Chief Scientist of Nursing and Midwifery
for the World Health Organization (WHO), overseeing policy on nursing and midwifery
services. She served for seven years in the PAHO/WHO Caribbean
Program Coordination Office in Barbados, assisting the ministries
of health with human resource planning, management, and training.
Organization (WHO), overseeing policy on nursing and midwifery
services. She served for seven years in the PAHO/WHO Caribbean
Program Coordination Office in Barbados, assisting the ministries
of health with human resource planning, management, and training.
Boufford is Professor of Public
Service, Health Policy, and Management at New York University.
She has served as Acting Assistant Secretary for Health in
the U.S. Department of Health and Human Services, as the U.S.
representative on the executive board of the World Health
Organization, and as director of the King's Fund College in London, a royal charity that supports health and
social services in the United Kingdom.
College in London, a royal charity that supports health and
social services in the United Kingdom.
Only three years after becoming
a physician, Nabarro was off to work as a district health
officer in East Nepal. Since then, he has worked in Southeast
Asia for Save the Children Fund and in Africa for the British
government's Overseas Development Administration. He
joined WHO in 1999 and in 2005 was appointed as the United
Nations Senior Coordinator for Avian and Human Influenza.
|
 |
| |
 |
|
|
|
| |
|
|
| |
| |
|
|
| |
The Global Government Chief Nursing Officers'
Institute, sponsored by Johnson & Johnson, focused specifically
on challenges facing CNOs. Held before the forum, it offered
a neutral and confidential forum for discussion. Several CNOs
were invited to offer lessons they had learned as a CNO. Jesmond
Sharples kindly permitted his to be published. |
|
| |
|
|
| |
Ten
Lessons I Have Learned as a CNO |
|
| |
By
Jesmond Sharples
CNO, Malta |
|
| |
|
|
| |
 1.
There is no chief without a tribe. 1.
There is no chief without a tribe.
2. There are
no black and white solutions, only gray ones.
3. There are
100 ways of how to do things right, but there is only one
way to do the right thing.
4. Don't
forget the lessons of the past by trying to look too much
into the future.
5. Being a CNO
involves the fine art of tightrope walking between politicians
and the associations without having a safety net to break
one's fall.
6. A CNO ought
to value humankind for what it is and not for what it ought
to be.
7. What you
think is definitely right might well be rightly wrong.
8. Don't
bother too much about whether a glass is half empty or half
full. Be more concerned with whose thirst that water is to
quench.
9. CNOs are
made, not born, but they do die.
10. Don't
forget your sense of humor. |
|
| |
|
|
|
|
| |
|
|
| |
|
|
| |
Reducing
the push-pull effect
Though
some developing countries are trying to improve salaries and working
conditions to keep nurses in-country, they are hampered by what
they cannot control: nursing shortages in developed countries. Shortages
in developed countries trigger a push-pull effect. Poor conditions
push nurses out of their home country, while developed countries
pull migrant nurses in to fill their own shortages. For many conference
participants, the question was, "Would nursing migration be
an issue if there were no shortages in developed countries?"
Part of the solution to the push-pull
effect lies in developing cooperative efforts by those countries
on the pulling side of the equation.
When Great Britain, for example, infused
funding into its national health care system in 2000, its leaders
recognized the top goal was to make the country more self-sufficient
in terms of its workforce. Health care leaders began working on
long-term plans to draw British nurses back into nursing and to attract new ones into the profession by fostering a better image
of the country's department of health. To address short-term
needs, they decided to recruit internationally, though only as a
temporary measure, says Debbie Mellor, director of workforce capacity
for the country's department of health. "We were very
concerned if we were going to increase international recruitment
that it be done ethically," she says.
to attract new ones into the profession by fostering a better image
of the country's department of health. To address short-term
needs, they decided to recruit internationally, though only as a
temporary measure, says Debbie Mellor, director of workforce capacity
for the country's department of health. "We were very
concerned if we were going to increase international recruitment
that it be done ethically," she says.
They
developed a voluntary code that independent providers and recruiters
had to sign if they wanted to work with the National Health Service.
The code included a list of "no-recruit" countries where
workforce shortages were especially grave. The code specified that
nurses could be imported from the Philippines and South Africa,
with specific memos of understanding signed with these countries.
"Our
experience in the U.K. is that partnerships can reduce the push
and pull factor," Mellor said. "The bilateral agreements
and programs of cooperation have been very useful and a helpful
way for us to make sure that we're proceeding in an ethical
way."
While
international recruitment was under way, the department also expanded
its number of training locations and promoted the National Health
Service as a model employer in a public campaign. A new, fairer
pay strategy was implemented, and child care needs of the nursing
workforce were addressed, as were issues of violence and harassment
in the workplace.
"We
had an 80% increase in U.K. nurses coming out of training and had
less of a need to rely on international recruitment," Mellor
said. "All of us in our health systems should be aiming for
greater self-sufficiency."
Likewise,
the Philippines began addressing its nursing shortage in a strategic
way, said nursing professor Marilyn Lorenzo, of the University of
the Philippines at Manila. While that country's leaders were
in the process of long-term planning for human resources in health
care, she came forward with data showing inadequate standards and
salary inequity among health care workers throughout the country.
The Philippine master plan for Human Resources for Health now addresses
national competency standards, the promotion of ethical recruitment,
and salary increases, and government nursing positions now outpace
those in the private sector. She told conference attendees that
the next step is to organize a network to implement the plan more
broadly, which over the next five years is expected to result in
an increase of health care workers working in underserved areas.
As
countries like Great Britain heed the call to action to fill their
own vacancies, poorer countries may get some relief from international
recruitment. And there are other positive changes as well, according
to Mireille Kingma, of the International Council of Nurses. Some
studies suggest that workers on average return to their home country
after five years. Additionally, job opportunities are improving
worldwide, especially for women.
But
real change in migration flows, Kingma said, will happen when poor
countries achieve benchmarks of development, such as clean water,
lowered infant and maternal mortality, and a thriving economy. In
that way, regardless of what happens in wealthy countries, developing
countries can start down the path to a self-sufficient workforce. |
|
| |
|
|
| |
| |
|
|
 |
Deploying
Data |
 |
| |
|
|
 |
 Any
health care system needs good management to grow its nursing
capacity—an issue Kenya is beginning to address with
the help of the School of Nursing. Kenya's Ministry
of Health lacked accurate data on the number of nurses in
the country. Every time a nurse went for training, a new form
was filled out and stored in a file according to the type
of training. A nurse's name could appear in numerous
files, making it nearly impossible to track an individual
nurse's training. The Centers for Disease Control and
Prevention, with the help of School of Nursing faculty, helped
Kenyan nurses design an electronic database that would assist
the country's health care leaders in workforce management
and policy. While the database is in only one province thus
far, project leaders hope soon to put workstations in Kenya's
seven other provinces. This is a welcome sign in a country
where some studies say that 5,000 nurses are unemployed, and
40% of the nursing positions are vacant because of the difficult
task of becoming registered after training is completed. Any
health care system needs good management to grow its nursing
capacity—an issue Kenya is beginning to address with
the help of the School of Nursing. Kenya's Ministry
of Health lacked accurate data on the number of nurses in
the country. Every time a nurse went for training, a new form
was filled out and stored in a file according to the type
of training. A nurse's name could appear in numerous
files, making it nearly impossible to track an individual
nurse's training. The Centers for Disease Control and
Prevention, with the help of School of Nursing faculty, helped
Kenyan nurses design an electronic database that would assist
the country's health care leaders in workforce management
and policy. While the database is in only one province thus
far, project leaders hope soon to put workstations in Kenya's
seven other provinces. This is a welcome sign in a country
where some studies say that 5,000 nurses are unemployed, and
40% of the nursing positions are vacant because of the difficult
task of becoming registered after training is completed. |
 |
| |
 |
|
|
|
| |
|
|
|
|
|