








|
 |
| |
 |
|
  |
 arly
in spring semester, when the air is still nippy and the dogwoods
have yet to bloom, Noelle delivers her babies with ease, her feet
in stirrups, her abdomen growing rigid with each contraction, her
cervix opening around the crown of the baby’s head. The deliveries
are textbook, and the babies perfectly arly
in spring semester, when the air is still nippy and the dogwoods
have yet to bloom, Noelle delivers her babies with ease, her feet
in stirrups, her abdomen growing rigid with each contraction, her
cervix opening around the crown of the baby’s head. The deliveries
are textbook, and the babies perfectly healthy. The junior nursing students who receive each baby under
the guidance of the faculty nurse-midwife carry the newborn to the
nearby warming bed with hidden sighs of relief and visible grins
of delight.
healthy. The junior nursing students who receive each baby under
the guidance of the faculty nurse-midwife carry the newborn to the
nearby warming bed with hidden sighs of relief and visible grins
of delight.
But as in real life, things are not
always so easy for the stoic mannequin. By the end of the semester,
her deliveries become longer and more difficult. The baby fails
to shift to the right birth position, and the umbilical cord becomes
wrapped around its neck. Noelle’s late spring babies arrive
with serious problems. Deprived of oxygen, their lips and fingers
slowly become cyanotic, setting off the code alert that brings the
now more advanced students racing to the bedside.
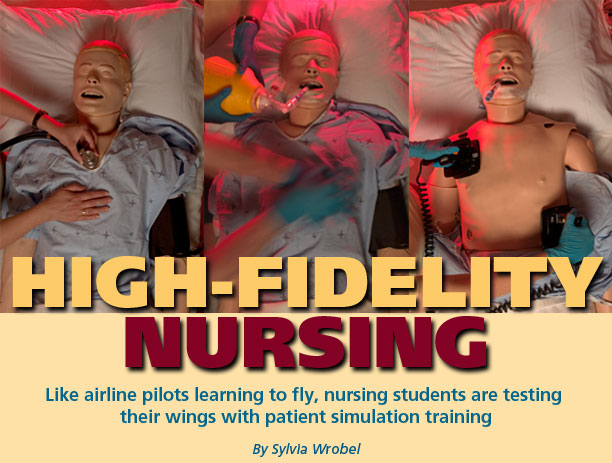
Noelle can deliver a baby every five
minutes if and when the nursing faculty need her to. But she is
only one of the life-size mannequins—officially known as high-fidelity
human patient simulators—helping revolutionize clinical education
in the Nell Hodgson Woodruff School of Nursing. Her older and even
more sophisticated brother, SimMan, has realistic heart and chest
sounds. His chest rises and falls with each breath, his pulses are
palpable, and he groans with pain, answers questions, and asks for
help. He—or she, with the quick addition of a wig, female
anatomy, and softer voice—is dependably unhealthy, suffering
whatever ailment and requiring whatever diagnosis and treatment
that undergraduate or graduate students need to learn.
When students meet SimMan shortly
after they enter nursing school, he usually has chest pain and difficulty
breathing. They painstakingly take his vital signs and history,
which he provides between wheezes, and study the monitor over his
head. By the time they are seniors, his problems have become more
critical—an undiagnosed pulmonary embolus, for example—and
so have the decisions they need to make. Wrong ones, or ones made
too slowly, and his respiration slows and eventually stops. “What
could we have done differently?” asks the supervising faculty
member. For the rest of their professional lives, faced with flesh-and-blood
patients with similar problems, the shocked students will remember
those answers.
For the rest of their professional lives, faced with flesh-and-blood
patients with similar problems, the shocked students will remember
those answers.
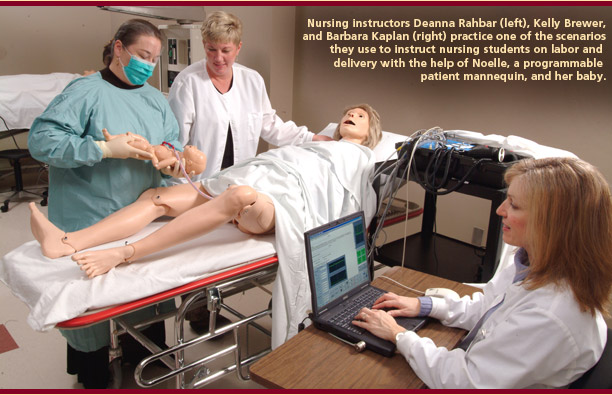
“These simulations become very
real to our students,” says Barbara Kaplan, coordinator of
the Charles F. and Peggy Evans Center for Caring Skills. No one
would mistake expressionless Noelle, her little baby with its protruding
umbilical cord, or SimMan with his injectable rubber arm patches,
for living, breathing humans. What quickens the students’
heartbeats, what makes them impulsively reach out to stroke the
mannequin’s arm in comfort, are the patient care scenarios
carefully planned and programmed by nursing faculty like Corrine
Abraham (for undergraduates), Julie Davey (for graduate students)
and Bethany Robertson (who developed the Noelle program) in collaboration
with Kaplan. |
  |
| |
 |
|
 |
| |
 |
|
  |
From
Learning to Doing
 imulation is the single most important trend in nursing education
today, the way to move from learning to doing,” says Darla
Ura, clinical associate professor of adult and elder health and
director of the Evans Center. Its use, she adds, is non-negotiable
in today’s health care environment. High patient acuity (seriousness
of disease on admittance) and compressed length of stay leave little
time for clinical education. A cholecystectomy patient who might
have spent a week or 10 days in the hospital when Ura entered practice
now has the operation on an outpatient basis or a 24-hour short
stay (most likely a laparoscopic procedure the surgeon first learned
using a virtual reality simulator). At the same time, nurses on
the medical-surgical unit or in the ICU are increasingly
imulation is the single most important trend in nursing education
today, the way to move from learning to doing,” says Darla
Ura, clinical associate professor of adult and elder health and
director of the Evans Center. Its use, she adds, is non-negotiable
in today’s health care environment. High patient acuity (seriousness
of disease on admittance) and compressed length of stay leave little
time for clinical education. A cholecystectomy patient who might
have spent a week or 10 days in the hospital when Ura entered practice
now has the operation on an outpatient basis or a 24-hour short
stay (most likely a laparoscopic procedure the surgeon first learned
using a virtual reality simulator). At the same time, nurses on
the medical-surgical unit or in the ICU are increasingly responsible for more tasks and sicker patients. Although senior
nursing students still have rotations through Emory and other area
hospitals, much of the hands-on learning most practicing nurses
acquired in clinical settings now must be taught in simulation laboratories.
responsible for more tasks and sicker patients. Although senior
nursing students still have rotations through Emory and other area
hospitals, much of the hands-on learning most practicing nurses
acquired in clinical settings now must be taught in simulation laboratories.
Changing the traditional “see
one, do one” method of teaching from human patients to simulated
ones gained further support after a hard-hitting Institute of Medicine
report focused on medical errors and how to reduce them (“To
Err Is Human: Building a Safer Health System,” 1999).
Whatever the reasons behind it, this
shift to simulation suits the nursing students just fine. Because
the patients aren’t real, even students early in their training
are allowed to become more involved in hands-on care, critical decision-making,
and teamwork. Like airline pilots crashing and burning repeatedly
as they “fly” in simulated cockpits, nursing students
can make mistakes without causing disasters. No one gets hurt from
errors in simulation, and students learn lessons that will benefit
them and their patients for the rest of their careers.
|
  |
| |
 |
|
  |
A
(simulated) hospital of its own
 lmost overnight, the Evans Center enabled the nursing school to
become the Woodruff Health Sciences Center’s biggest user
of high-fidelity mannequins.
lmost overnight, the Evans Center enabled the nursing school to
become the Woodruff Health Sciences Center’s biggest user
of high-fidelity mannequins.
The use of such technology had not
been an option in the nursing school’s former building (located
on Asbury Circle behind Emory University Hospital), which wasn’t
wired adequately for students even to operate an electric hospital
bed and where the only life-size “care dolls” (less
realistic models used for changing dressings, setting casts, and other tasks) had no flexible joints, much less pulses and voices.
In the late 1990s, a grant from the Helene Fuld Health Trust made
possible the purchase of more realistic mannequins, ones with veins
in which an IV could be started, patches for injections (saving
hundreds of oranges used for practice each year), and programmable
heart and breath sounds. Ura and other faculty began visiting sister
nursing schools where simulation was already taking off and compiled
the school’s “must have” shopping list in hopes
that if they planned well, the money would come.
other tasks) had no flexible joints, much less pulses and voices.
In the late 1990s, a grant from the Helene Fuld Health Trust made
possible the purchase of more realistic mannequins, ones with veins
in which an IV could be started, patches for injections (saving
hundreds of oranges used for practice each year), and programmable
heart and breath sounds. Ura and other faculty began visiting sister
nursing schools where simulation was already taking off and compiled
the school’s “must have” shopping list in hopes
that if they planned well, the money would come.
Miraculously, it did. As the nursing
school prepared to move into its new building on Clifton Road in
December 2000, the school learned that the late Charles and Peggy
Evans, who built an automobile sales enterprise in the Atlanta area,
had bequeathed Emory a multimillion dollar gift in appreciation
for the medical and nursing care they received before their deaths.
What better way to honor their generosity and memory than to build
a center where such caring skills could be taught? (A large portion
of their gift also is being used by the medical school for a new
education building and programs.)
Already twice renovated to expand
size and technology, the Evans Center includes a small hospital
ward, with eight beds separated by privacy curtains. Until recently,
ever-pregnant Noelle stayed in another spacious room near the ward
with her newborn. Two SimMan mannequins kept her company, along
with other life-size children and adult mannequins, care dolls,
and numerous simulated body parts, such as the shoe box-size pelvis
on which students learn catheterization. Computers spit out realistic
laboratory results and X-rays.
In May, the first Emory BSN students
with two years of simulation training graduated, entering nursing
practice with unprecedented experience and greater confidence in
a wide range of clinical situations. This summer, the Evans Center
added an observation and control room (where Noelle and SimMan now
reside) with one-way mirrors, video cameras, and enhanced technology.
In September, an ongoing teaching partnership between nursing and
medicine was expanded as fourth-year medical students and nursing
seniors began working together in the Evans Center to learn how
to respond as a team in a medical emergency.
|
  |
| |
 |
|
 |
| |
 |
|
  |
Playing
well with others
 he
School of Nursing is well on its way to becoming a national leader
in simulation training, according to Dr. Carol Fowler Durham, a
simulation expert at the University of North Carolina School of
Nursing. When Durham came to Emory to give the 2004 he
School of Nursing is well on its way to becoming a national leader
in simulation training, according to Dr. Carol Fowler Durham, a
simulation expert at the University of North Carolina School of
Nursing. When Durham came to Emory to give the 2004 David Jowers Lecture and conduct a simulation workshop for nursing
faculty, she was impressed by the high-tech Evans Center and the
faculty’s enthusiasm and eagerness to use simulation. In many
ways, especially in terms of teamwork between the medical and nursing
schools, the school is “way ahead of the game,” she
says.
David Jowers Lecture and conduct a simulation workshop for nursing
faculty, she was impressed by the high-tech Evans Center and the
faculty’s enthusiasm and eagerness to use simulation. In many
ways, especially in terms of teamwork between the medical and nursing
schools, the school is “way ahead of the game,” she
says.
Last year, the School of Nursing and
the School of Medicine jointly recruited Dr. Martin Reznek, a highly
experienced expert in simulation training for medicine and nursing,
to expand simulation training opportunities for students in both
fields.
“Emergency medicine is a great
field for this kind of collaborative training,” says Reznek,
an assistant professor in the School of Medicine. “When a
patient arrives in the ER, there are always more tasks than one
person can do, forcing quick decisions and delegation of responsibilities.
Nurses and physicians interact in crisis situations all day long,
and the physician/nurse hierarchy is not as firmly established as
in some fields.”
Reznek’s tasks include expanding
simulation programs for nursing and medical students and bringing
in grants to the nursing school. The new class that began in September—“Learning
in Interdisciplinary Teams Makes Us Safer” (LITMUS)—does
both, having won an educational grant from the university.
In LITMUS, groups of two medical students
and two nursing students listen to lectures about the different
tasks that need to be done in specific medical crises and how physicians and nurses
work together to get those tasks done quickly and correctly.
be done in specific medical crises and how physicians and nurses
work together to get those tasks done quickly and correctly.
The simulation begins when a code
sounds, and the four students crowd around a bed where SimMan is
in programmed peril. As in the real ER, they don’t know what
to expect. The case may be a cardiac arrhythmia that has turned
into cardiac arrest. Or it may involve the altered mental status
of head trauma. “Part of the art form of developing simulations,”
says Reznek, “is to match what students know intellectually
and what they need to know operationally.”
Whatever the case, learning to respond
as a team is the primary imperative. That’s not easy to learn
in the simulation’s crisis atmosphere and with two different
professional cultures and four personalities around the bedside.
But it is a lot easier—and a lot safer, as the course title implies—than trying to learn it for the first time around
the bedside of a barely living patient. And it will give students
an early chance to discover the strengths of each other’s
profession.
implies—than trying to learn it for the first time around
the bedside of a barely living patient. And it will give students
an early chance to discover the strengths of each other’s
profession.
After the simulation ends, the faculty
undertake the most important step—debriefing. Students watch
their simulation on videotape made in the Evans Center’s new
control room and answer two questions that open each session: What
did you do well? What could you have done better?
More steps are in store for faculty,
says Reznek. Using the videotapes, they can hone the scenarios and
curriculum to improve team interaction and conduct research on the
effectiveness of simulation and its impact on patient safety. Other
research may focus on whether doctors and nurses have different
perceptions of what is important for patient care that may affect
how well they work as a team.
|
  |
| |
 |
|
  |
Simulation,
synthesis, and the making of a nurse
 xuberant
students often claim they learned more in an hour in the simulation
laboratory than they learned all semester. Their instructors just
smile. They know the real strength of simulation is to show students
the effects of the pathophysiology they have been studying and to
synthesize theory into practice. They also know that moment of synthesis
is both an emotionally and intellectually powerful experience that
helps students become better nurses more quickly. xuberant
students often claim they learned more in an hour in the simulation
laboratory than they learned all semester. Their instructors just
smile. They know the real strength of simulation is to show students
the effects of the pathophysiology they have been studying and to
synthesize theory into practice. They also know that moment of synthesis
is both an emotionally and intellectually powerful experience that
helps students become better nurses more quickly.
Kaplan tells of a senior nursing student
who was crestfallen after her first simulation with a code, the
alarm that sounds when a patient turns critical. “I was awful,”
she said, near tears. “How will I ever learn enough?”
The next week, during her hospital
rotation, the patient with whom she was talking suddenly lost consciousness.
The student called the code, grabbed the crash cart, placed a board
under the patient in preparation for defibrillation/compression,
and began CPR. “I knew what to do,” she later told Kaplan
gleefully.
SimMan (and the nursing faculty) had
done it once again.
Sylvia
Wrobel is the former associate vice president for health sciences
communications and a frequent contributor to Emory’s health
sciences publications.
|
  |
| |
 |
|
|
|
|